
Factors affecting laryngectomy rate during the COVID-19 pandemic
Introduction
Head and neck cancer constitutes 3.4% of Australian cancer diagnoses with an incidence of 16.8 per 100,000. Pharyngeal and laryngeal cancer are the second and third most common subgroups at 3.2 and 2.6 per 100,000, respectively (1). Treatment varies greatly depending on staging and airway function. While less advanced tumours are amenable to transoral surgery or targeted radiotherapy, advanced disease requires intensive therapy to achieve locoregional control. Laryngeal preservation treatments are now preferred for less advanced disease and historically favoured laryngectomy is recommended only for T4 disease, laryngeal dysfunction or as salvage for recurrent disease (2-4). Early diagnosis and expedient treatment are therefore critical in managing patients with single modality care to reduce morbidity and mortality.
The coronavirus disease 2019 (COVID-19) resulted in significant disruptions to the delivery of healthcare in Australia, and Victoria particularly. Public health orders and city-wide lockdowns reduced patient mobility and decreased access to primary care, which combined with anxiety surrounding transmission reduced patient engagement with healthcare. Healthcare institutions were similarly limited in outpatient capacities, investigation facilitation and provision of sufficient elective operating lists (5,6). Clinicians faced ethical dilemmas of providing timely, essential care while mitigating exposure risk to patients and team members—magnified among otolaryngologists who regularly perform aerosol-generating procedures (AGPs) in daily practice (7).
Early in the pandemic, clinicians involved in cancer management raised concerns about the potential for these factors to precipitate delayed diagnosis, loss to follow up and stage migration. International teams investigating the effects of the pandemic on laryngeal cancer staging found mixed results with some demonstrating higher proportions of advanced stage disease and larger tumour volume during the pandemic (8-10), while others found no such differences (11). Locally, a study performed in regional Victoria found no difference in time from referral to first appointment or treatment, with no significant differences in proportions of advanced stage disease among all patients referred with head and neck cancer more generally (6). Anecdotal observation of increased laryngectomies performed at our hospital during the pandemic prompted exploration of the possible impact of the COVID-19 on patients receiving treatment for laryngeal cancer within this tertiary metropolitan referral centre.
Methods
Study design and research ethics
This retrospective review assesses the impact of the COVID-19 pandemic upon timing of presentation of laryngeal and pharyngeal malignancies and therefore laryngectomy rates at Austin Health. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by the Austin Health Human Research Ethics Committee (ERM 86873). Because of the retrospective nature of the research, the requirement for informed consent was waived. The study is reported according to the STROBE reporting guidelines (1) (available at https://www.theajo.com/article/view/10.21037/ajo-24-35/rc).
Participants
The Austin Health network services approximately 1.28 million people in a catchment including eight shires and the rural cities Mildura and Bendigo. Patients diagnosed with laryngeal or hypopharyngeal primary malignancies who underwent total laryngectomy (TL) or laryngopharyngectomy (LP) at Austin Health between December 1st, 2016 and September 1st, 2023 were eligible for inclusion. Patients with non-squamous cell malignancies were excluded. No age or gender exclusions were necessary. Pre- and post-operative tumour staging were determined at the Austin Health Head and Neck Cancer multi-disciplinary meeting (MDM) in accordance with American Joint Committee on Cancer (AJCC) guidelines. The AJCC system is utilised to stage malignancies, estimate prognosis and guide consistent selection of best treatment for individual patients. MDM recommendations were also given regarding eligibility for surgical, adjuvant chemotherapy (CTx) and radiotherapy (RTx) treatments.
Data acquisition
Data were accessed from the electronic and scanned electronic medical record (EMR) of Austin Health between January 2022 and September 2023.
Pandemic data
Participants were stratified based upon surgical treatment date. ‘Pre-pandemic’ patients were defined as TL/LP surgical management between December 1st, 2016 and December 31st, 2019, ‘pandemic’ patients as January 1st, 2020 to January 31st, 2022 and ‘post-pandemic’ patients as February 1st, 2022 to September 1st, 2023.
Participant characteristics
Participant characteristics were reported using descriptive statistics and included demographic features, social history and comorbidities. Disease characteristic data included primary cancer site and tumour-node (TN) staging. Features of treatment included definitive and adjuvant oncological interventions, primary procedure type as well as any additional procedures. Timing between key events (e.g., referral to appointment) were collected from EMR. Where exact date could not be determined, shortest duration was utilised e.g., “hoarseness since January” was taken as January 30th. ‘Salvage’ is defined as laryngectomy performed following RTx/CTx with curative intent, usually in context of locoregional recurrence. Patients who underwent salvage laryngectomy or who had undergone workup at another tertiary centre were excluded from these analyses.
Statistical analysis
Participant data were managed using Microsoft Excel software with randomly assigned participant number for identification. Statistical analysis utilised inbuilt Microsoft Excel statistical software (12). Categorial variables were reported as frequencies/percentages [n (%)]. Continuous variables were reported as mean and median, normal distribution was not assumed. One-way analysis of variance (ANOVA) analysis and Chi-squared goodness of fitness test (χ2) were utilised to analyse demographic differences across strata. Mann-Whitney U test (U) was utilised for comparison of means, Fisher’s exact test (Pb) was utilised to determine association between strata and TN staging. All tests were two-tailed with P≤0.05 denoting statistically significant association.
Results
Participant demographics and comorbidities
Between December 2016 and August 2023, 28 patients underwent either TL or LP at Austin Health and their records were reviewed retrospectively. Eleven/28 patients (39%) were stratified as pre-pandemic, 13 (46%) as pandemic, and 4 (14%) as post-pandemic (Table 1). Demographic characteristics and comorbidities are demonstrated in Table 1. In total, 93% of patients were male (n=26) and 7% were female (n=2), mean age at surgical treatment date was 71 years [standard deviation (SD), 63–78]. Most patient’s history included squamous cell carcinoma (SCC) risk factors of cigarette smoking (n=24, 86%) or heavy alcohol use (n=12, 43%).
Table 1
| Demographics | Pre-pandemic (n=11) | Pandemic (n=13) | Post-pandemic (n=4) |
|---|---|---|---|
| Gender | |||
| Female | 0 [0] | 1 [8] | 1 [25] |
| Male | 11 [100] | 12 [92] | 3 [75] |
| Age at Dx (years) | |||
| 51–60 | 2 [18] | 2 [15] | 1 [25] |
| 61–70 | 4 [36] | 3 [23] | 2 [50] |
| 71–80 | 5 [46] | 8 [62] | 1 [25] |
| Smoking Hx | |||
| No | 3 [27] | 1 [8] | 0 [0] |
| Yes | 8 [73] | 12 [92] | 4 [100] |
| Alcohol use | |||
| Heavy | 2 [18] | 9 [69] | 1 [25] |
| Not heavy | 3 [27] | 1 [8] | 2 [50] |
| Nil/UTA | 6 [55] | 3 [23] | 1 [25] |
| Comorbidities | |||
| Hypertension | 5 [45] | 5 [38] | 1 [25] |
| Dyslipidaemia | 3 [27] | 3 [23] | 0 [0] |
| Gastro-oesophageal reflux disease | 1 [9] | 0 [0] | 1 [25] |
| Type 2 diabetes mellitus | 1 [9] | 0 [0] | 0 [0] |
| Ischaemic heart disease | 1 [9] | 3 [23] | 1 [25] |
Data are presented as n [%]. Alcohol use was characterised as ‘heavy’ if ≥15 standard drinks per week or ‘not-heavy’ if 1–14 standard drinks per week (12). Dx, diagnosis; Hx, history; UTA, unable to ascertain.
Pandemic data
The rate of TL/LP surgeries performed during the pandemic was notably higher at 6.5 per year, compared to 3.5 and 2.5 in the pre- and post-pandemic periods respectively. There was no significant difference in patient demographics or incidence of risk factors between pandemic strata.
Disease characteristics
Comparison of primary malignancy site and intervention rates between strata are given in Figure 1. The larynx was the most common site of primary malignancy in both the pre- and post-pandemic strata (64%, n=7; and 75%, n=3, respectively), however, during the pandemic the majority of patients presented with malignancy of multiple upper aerodigestive tract structures (38%, n=5).
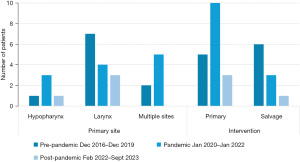
Prior to the pandemic, salvage procedures were performed more frequently (55%, n=6) than primary laryngectomy (45%, n=5). During and post-pandemic the proportion of salvage laryngectomies procedures was lower (23%, n=3; and 25%, n=1, respectively), though this decline did not represent a statistically significant difference between strata (χ2=0.24; P=0.88).
Comparison of resection T-staging assessments between pandemic strata are demonstrated in Figure 2. A proportional increase in the number of patients presenting with high stage (T4a/b) malignancies in the pandemic and post-pandemic groups (54%, n=7; and 75%, n=3, respectively) compared to pre-pandemic (45%, n=5) is demonstrated (χ2=0.77; P=0.38).
Treatment
A shift away from definitive chemo/radiotherapy (CRTx) treatments and towards primary surgical intervention is demonstrated during the pandemic and post-pandemic periods, as illustrated in Table 2. The rate of LP compared to TL procedures also rose from just 18% (n=2) pre-pandemic to 54% (n=7) during the pandemic, though this was not statistically significant (χ2=3.4; P=0.18). It is worth noting that a number of patients in the pandemic and post-pandemic group were recommended for adjuvant CRTx but were too unwell to receive this treatment. A significant rise in prevalence of concurrent neck dissections was also demonstrated in the pandemic and post-pandemic groups (85%, n=11; and 100%, n=4, respectively), compared to pre-pandemic (45%, n=5) (χ2=6.34; P=0.01).
Table 2
| Treatment | Pre-pandemic (n=11) | Pandemic (n=13) | Post-pandemic (n=4) |
|---|---|---|---|
| Definitive (failed) | |||
| RTx | 6 [55] | 3 [23] | 1 [25] |
| CTx | 0 [0] | 3 [23] | 1 [25] |
| Adjuvant | |||
| RTx | 3 [27] | 8 [62] | 2 [50] |
| CTx | 5 [45] | 3 [23] | 1 [25] |
| Primary procedure | |||
| TL | 9 [82] | 6 [46] | 2 [50] |
| LP | 2 [18] | 7 [54] | 2 [50] |
| Additional procedures | |||
| Neck dissection | 5 [45] | 11 [85] | 4 [100] |
| Bilateral | 3 | 10 | 4 |
| Unilateral | 2 | 1 | 0 |
| Free flap | 1 [9] | 3 [23] | 2 [50] |
| Thyroidectomy | 1 [9] | 0 [0] | 2 [50] |
| Hemithyroidectomy | 5 [45] | 6 [46] | 1 [25] |
| Oesophagectomy | 0 [0] | 3 [23] | 1 [25] |
| Pre-op tracheostomy | 0 [0] | 3 [23] | 1 [25] |
| Tracheoesophageal puncture | 10 [91] | 8 [62] | 3 [75] |
| Primary | 8 | 8 | 3 |
| Secondary | 2 | 0 | 0 |
Data are presented as n [%] or n. RTx, radiotherapy; CTx, chemotherapy; TL, total laryngectomy; LP, laryngopharyngectomy.
Timing
Differences in timing between key workup and treatment events between strata are illustrated in Figure 3. Average time between symptom onset and general practitioner (GP) review was substantially higher during the pandemic at 215 days, compared to 52 days pre-pandemic and 32 days post-pandemic. Average time from referral to ENT appointment lengthened significantly from less than 1 week pre-pandemic, to approximately a month during the pandemic and almost 2 months in its wake. Once connected with ENT, both average time to biopsy and surgery were lower during the pandemic and have fallen further post-pandemic.

Discussion
On the 16th of March 2020, Victoria declared a ‘State of Emergency’, following the declaration of a pandemic by the World Health Organisation. Restrictions were imposed from March 2020 until February 2022 and included strict limitations to travel distance, gathering sizes, as well as mandatory quarantine following even potential exposures to the virus. The COVID pandemic temporally changed healthcare delivery over this period. Each Australian state had individualised implementation of lockdown in both duration and level of restriction to community and healthcare—making both the COVID experience and laryngectomy data heterogeneous and challenging to be directly compared.
For head and neck cancers, it is unclear whether these health restrictions precipitated delays in presentation or if patients presented with more advanced disease during this time. Noel et al. [2021] found no difference in amount of laryngectomies performed or stage of disease presentation in the first 6 months of the pandemic in the USA (11). Flores et al. (13) concluded that patients were hesitant to seek care during the pandemic, which resulted in more substantial nodal disease in 61 cases of head and neck SCC. Similarly, Akbari et al. (9) found that in Iraq, there was a statistically significant increase in nodal stage and tumour volume during a 1-year period during the pandemic compared to previous observations.
A study by Kiong et al. (14) conducted in the pandemic’s early stages found less head and neck cancers were diagnosed, however, they were on average larger with more advanced T-staging, suggesting patients were presenting for primary assessment later. This contradicts Heckel et al. (15) who demonstrated that of 706 patients there was no laryngeal malignancy advancement during the pandemic. Balk et al. (16) similarly showed no increased tumour or nodal disease burden during the pandemic but did report a higher rate of metastases in the pre-COVID era. Given these studies weren’t specifically examining laryngeal carcinomas nor under the same restrictions as Victoria, clear conclusions cannot be drawn.
Within this study population, we found that the time from first appointment with our Ear, Nose, and Throat (ENT) service to the time of biopsy decreased from 7.8 to 7.5 days during the pandemic. Additionally, median time from biopsy to surgery decreased from 34 to 24 days. This is concordant with the findings of Heckel et al. (15) who reported that treatment initiation time for head and neck cancers was decreased during the pandemic compared to prior (17). Heimes et al. (17) also demonstrated a reduction in the commencement of definitive management for oral cancers.
During the 2 years of the pandemic, Austin Health completed more laryngectomies than in the previous 4 years combined. Of the eleven laryngectomies pre-pandemic, five were primary procedures, compared to 10 during the pandemic. In the 18 months following the pandemic period, the number of laryngectomies performed decreased to four, of which three were primary procedures. This decrease in total number of laryngectomies does circumstantially support the observation that patients presented with more advanced laryngeal malignancy during the pandemic. Additionally, prior to the pandemic, the percentage of patients who underwent laryngectomy for T4 disease was 45%, compared to 54% during the pandemic. This supports our observation that patients presented with more advanced primary disease during the pandemic.
Prior to the pandemic, average symptom duration reported by patients at GP review was 52 days, which increased to 215 days during the pandemic. Following the pandemic period, this number reduced to 32 days. We cannot speculate what weight this delay in presentation had on oncological stage at presentation however, it is worthy of consideration as a potential cause.
This observed delay in presentation is thought to relate to laryngeal carcinomas being a largely ‘unseen’ carcinoma of the head and neck that aren’t readily examinable by the primary care physician without specialised equipment such a flexible nasal endoscopy—a risk in itself as a GP. Additionally, simple imaging modalities available to primary care physicians such as ultrasound and computer tomography (CT) may not readily detect early abnormalities. The symptoms common in laryngeal carcinomas such as persistent, progressive dysphonia, cough and stridor were exclusion criteria for presenting to a primary care physician during the pandemic. When coupled with government health department mandated restriction of movement and self-quarantine measures in those exposed or with symptoms, this could have contributed to observed delay in presentation to primary health care.
There was also variation between average time pre-pandemic (6 days), intra-pandemic (32 days) and post-pandemic (64 days) from referral to appointment which may have added to the overall delay. Prior to the pandemic, patients who eventually underwent laryngectomy were seen within an average of 1 week from receipt of referral, compared to a 1 month wait during the pandemic and over 2 months in the aftermath. We explain these findings in part due to constraints placed on health service workers in the setting of the pandemic and the restrictions particular to Victoria. There was a distinct effort in all public hospitals to reduce face-to-face outpatient clinic numbers with a reliance on telehealth in an effort to reduce the spread of the virus and protect medical, nursing and administration staff. Despite reversal of the most stringent restrictions in March of 2022, service delivery did not return immediately to ‘pre-pandemic standards’ and the healthcare system in Victoria remains overburdened by a backlog of referrals.
This study does have a number of limitations. It is estimated that only around 60 laryngectomies occur per year in Victoria, allowing only 28 patients to analyse over 6 years at Austin Health. This finite number of datapoints makes broad generalisation of this analysis challenging. One of the aims of this study was to examine if the COVID-19 pandemic resulted in patients seeking help from a medical practitioner later, and if this in turn meant that they were diagnosed with more advanced disease on presentation. However, lack of a centralised database of laryngectomies in Victoria necessitates reliance on retrospective qualitative measures such as patient/GP recall of symptom onset, rather than quantifiable measures and is therefore likely to be less accurate. Creation of a centralized database of laryngectomies in Victoria and/or Australia would be essential in advancing research in this field.
Our study suggests that advanced laryngeal cancer observed during the pandemic, was most likely due to a delay in treatment occurring at a primary health level. Service delivery at tertiary centres also remains insufficient to meet the backlog of demand in the wake of the pandemic. This highlights the importance of further research evaluation of service delivery at both primary and tertiary levels in understanding the impact of policy changes and crisis resource allocation on healthcare diagnoses and outcomes. Given the uniqueness of each Australian state restrictions throughout the pandemic, a future study providing comparison of numbers would provide a more granular analysis of the impact of COVID on healthcare systems.
Acknowledgments
We would like to thank the patients whose data contributed to this study. Our abstract has been accepted for poster presentation at the 74th ASOHNS Annual Scientific Meeting, Perth, Australia, taking place between the 8th and 10th of March, 2024.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://www.theajo.com/article/view/10.21037/10.21037/ajo-24-35/rc
Data Sharing Statement: Available at https://www.theajo.com/article/view/10.21037/ajo-24-35/dss
Peer Review File: Available at https://www.theajo.com/article/view/10.21037/ajo-24-35/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://www.theajo.com/article/view/10.21037/ajo-24-35/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by the Austin Health Human Research Ethics Committee (ERM 86873). Because of the retrospective nature of the research, the requirement for informed consent was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Australian Institute of Health and Welfare. Head and neck cancers in Australia. 2014. Available online: https://www.aihw.gov.au/getmedia/bdccebf2-dbe6-44e2-9104-8461d7e7c165/16933.pdf.aspx?inline=true
- Forastiere AA, Ismaila N, Lewin JS, et al. Use of Larynx-Preservation Strategies in the Treatment of Laryngeal Cancer: American Society of Clinical Oncology Clinical Practice Guideline Update. J Clin Oncol 2018;36:1143-69. [Crossref] [PubMed]
- Grover S, Swisher-McClure S, Mitra N, et al. Total Laryngectomy Versus Larynx Preservation for T4a Larynx Cancer: Patterns of Care and Survival Outcomes. Int J Radiat Oncol Biol Phys 2015;92:594-601. [Crossref] [PubMed]
- Rosenthal DI, Mohamed AS, Weber RS, et al. Long-term outcomes after surgical or nonsurgical initial therapy for patients with T4 squamous cell carcinoma of the larynx: A 3-decade survey. Cancer 2015;121:1608-19. [Crossref] [PubMed]
- Stevens MN, Patro A, Rahman B, et al. Impact of COVID-19 on presentation, staging, and treatment of head and neck mucosal squamous cell carcinoma. Am J Otolaryngol 2022;43:103263. [Crossref] [PubMed]
- Tan H, Preston J, Hunn S, et al. COVID-19 did not delay time from referral to definitive management for head and neck cancer patients in a regional Victorian centre. ANZ J Surg 2021;91:1364-8. [Crossref] [PubMed]
- Brody RM, Albergotti WG, Shimunov D, et al. Changes in head and neck oncologic practice during the COVID-19 pandemic. Head Neck 2020;42:1448-53. [Crossref] [PubMed]
- Elibol E, Koçak Ö, Sancak M, et al. The effect of COVID-19 pandemic on laryngeal cancer in a tertiary referral center. Eur Arch Otorhinolaryngol 2022;279:1431-4. [Crossref] [PubMed]
- Akbari M, Motiee-Langroudi M, Heidari F, et al. Impact of the COVID-19 pandemic on the stage and the type of surgical treatment of laryngeal cancer. Am J Otolaryngol 2022;43:103319. [Crossref] [PubMed]
- Solis RN, Mehrzad M, Faiq S, et al. The Impact of COVID-19 on Head and Neck Cancer Treatment: Before and During the Pandemic. OTO Open 2021;5:2473974X211068075.
- Noel CW, Li Q, Sutradhar R, et al. Total Laryngectomy Volume During the COVID-19 Pandemic: Looking for Evidence of Stage Migration. JAMA Otolaryngol Head Neck Surg 2021;147:909-11. [Crossref] [PubMed]
- Microsoft Excel. Microsoft Corporation. 2021.
- Flores CER, de Almeida DO, Freitas LVD, et al. Diagnosis of head and neck squamous cell carcinoma during the COVID-19 pandemic: a retrospective case-control study. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology 2023;136:e51. [Crossref]
- Kiong KL, Diaz EM, Gross ND, et al. The impact of COVID-19 on head and neck cancer diagnosis and disease extent. Head Neck 2021;43:1890-7. [Crossref] [PubMed]
- Heckel S, Bohr C, Meier J, et al. Head and neck oncology management in the time of COVID-19: results of a head and neck cancer center. J Cancer Res Clin Oncol 2023;149:12081-7. [Crossref] [PubMed]
- Balk M, Rupp R, Craveiro AV, et al. The COVID-19 pandemic and its consequences for the diagnosis and therapy of head and neck malignancies. Eur Rev Med Pharmacol Sci 2022;26:284-90. [PubMed]
- Heimes D, Müller LK, Schellin A, et al. Consequences of the COVID-19 pandemic and governmental containment policies on the detection and therapy of oral malignant lesions—a retrospective, multicenter cohort study from germany. Cancers 2021;13:2892. [Crossref] [PubMed]
Cite this article as: Elkington O, Webb H, Woliansky J, Rowe D. Factors affecting laryngectomy rate during the COVID-19 pandemic. Aust J Otolaryngol 2025;8:1.



