
Ear examination skills: a cross-sectional survey study of Australian junior doctors
Introduction
Otoscopy, clinical examination of the external auditory canal and tympanic membrane using an otoscope, is a basic clinic competency required to assess for ear pathologies. Otolaryngological problems account for up to 1 in 8 primary care presentations and 29% of overall paediatric presentations, and is therefore a commonly employed skill (1).
Ear-related disease is a common issue that junior doctors will encounter during hospital and community rotations. In 2022–2023, there were 113,761 ear and mastoid presentations (ICD-10-AM) to emergency departments across Australia, accounting for 13% of all presentations (2). All Australian medical graduates are required to undertake an emergency medicine rotation, exposing them to ear-related presentations requiring otoscopy.
Outside of ENT surgery and emergency medicine, competent otoscopy is a fundamental skill in general practice and paediatric medicine. A recent Australian Delphi method paper found that 92.6% of experts agreed competence in otoscopy should be a mandatory procedural skill for Australian medical graduates (3). However, other studies have found that recent medical graduates lack confidence in otoscopy and felt that more exposure was required (4,5). Structured otoscopy teaching has been linked to increased confidence in identifying anatomical landmarks and pathology when performing otoscopy (6,7).
The objective of this study is to analyse Australian junior doctors’ ability to identify anatomical landmarks and pathology on otoscopy, as well as interpret tuning fork tests and audiograms. We present this article in accordance with the STROBE reporting checklist (available at https://www.theajo.com/article/view/10.21037/ajo-24-37/rc).
Methods
A cross-sectional survey study was performed with responses collected between March to May of 2023 using Survey Monkey (8). The survey link and QR code were sent to education officers at New South Wales (NSW) and Australian Capital Territory (ACT) hospitals for distribution at intern and resident teaching sessions or via email. All responses were included for data collection. The primary objective was to capture a reflective sample of otology examination skills amongst junior doctors. The secondary objective was to analyse the presence of a relationship between confidence in otology examination and ENT exposure during medical school or in post-graduate training.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) with implied consent from all individual participants. The project was reviewed by the Northern NSW Local Health District Research Office under a non-Human Research Ethics Committee (HREC) pathway for low-risk projects and was deemed to be consistent with the principles and values outlined in the National Statement on Ethical Conduct in Human Research (2007). As a low-risk survey project, exemption was granted from HREC approval, in line with NSW Health policy.
Data collected included current post-graduate year, amount of ENT experience in medical school and as a junior doctor, self-reported confidence in otoscopy, ability to identify anatomy of a normal ear, ability to identify basic pathology on otoscopy, self-reported confidence in interpreting audiograms, accuracy of audiogram interpretation, ability to interpret tuning fork tests, and whether respondents felt more ENT exposure was needed during medical school or post-graduate training. Assessment of ability to identify basic ear anatomy, identify pathology, interpret audiograms and tuning fork tests was achieved through multiple-choice questions (Table 1 and Appendix 1) (9-11). Likert scales were used to assess self-reported confidence in otology examination.
Table 1
| Domain assessed | Respondents asked to identify |
|---|---|
| Anatomy | Malleus, light reflex, attic, annulus |
| Pathology | Acute otitis media, otitis media with effusion, tympanic membrane perforation, cholesteatoma, haemotympanum, extruded middle ear ventilation tube |
| Audiograms | Normal hearing, conductive hearing loss, sensorineural hearing loss, mixed hearing loss |
| Tuning Fork Tests | Normal tuning fork test, right sided conductive hearing loss |
Statistical analysis was completed via R Studio (12). Univariate analysis presented as odds ratios were used when comparing multiple variables. Two-sided P values were calculated using mid-p exact test for discrete variables with count data less than ten. A P value less than 0.05 was considered statistically significant.
Results
There were 83 responses from 828 survey distributed, with a response rate of 10%. There were 42 responses from interns, 22 responses from residents and 22 from doctors with three or more years of post-graduate experience. Of the respondents, 71% (n=59) had less than one week of ENT experience during medical school (Figure 1). In terms of post-graduate ENT experience, almost three-quarters of junior doctors surveyed (71%, n=59) had no experience, 23% (n=19) had four weeks or less, and 6% (n=5) had between five to twelve weeks.
Of the respondents, 65% (n=54) were not confident at all or slightly confident in their ability to perform otoscopy and accurately describe their findings. Only 10% (n=8) of the junior doctors could correctly identify all anatomical structures on otoscopy. Half of the survey respondents (49%, n=41) correctly identified all pathologies present on otoscopy. Of the respondents, 90% (n=75) self-reported no confidence or slight confidence in their ability to interpret an audiogram. Almost half of those surveyed (45%, n=37) could correctly interpret tuning fork tests and 29% (n=24) correctly identified all patterns of hearing on audiograms (Table 2). Almost all junior doctors surveyed (94%, n=78) agreed or strongly agreed that more ENT exposure during medical school or post-graduate training would be useful.
Table 2
| Ear examination domain | Number of respondents correctly identifying on survey |
|---|---|
| Anatomical structures | 8/83 (10%) |
| Pathology | 41/83 (49%) |
| Tuning Fork Tests | 37/83 (45%) |
| Audiogram | 24/83 (29%) |
Comparing respondents with more than one week of ENT teaching during medical school to those with less than or equal to one week, there was no significant difference in ability to correctly identify anatomy (OR 1.6, 95% CI: 0.3–7.2; P=0.59), identify pathology (OR 1.3, 95% CI: 0.5–3.5; P=0.59) interpret audiograms (OR 1.0, 95% CI: 0.3–2.9; P=0.96) and interpret tuning fork tests (OR 1.4, 95% CI: 0.5–3.6; P=0.54) (Table 3, Figure 2).
Table 3
| Ear examination domain | Correct answers (≤1 week ENT teaching during medical school) | Correct answers (>1 week ENT teaching during medical school) | Odds ratio (95% CI) (>1 week ENT teaching) | P value |
|---|---|---|---|---|
| Anatomy | 5/59 (8.5%) | 2/24 (8.3%) | 1.6 (0.3–7.2) | 0.59 |
| Pathology | 28/59 (47.5%) | 13/24 (54.2%) | 1.3 (0.5–3.5) | 0.59 |
| Audiograms | 17/59 (28.8%) | 7/24 (29.2%) | 1.0 (0.3–2.9) | 0.96 |
| Tuning Fork Tests | 25/59 (42.4%) | 12/24 (50%) | 1.4 (0.5–3.6) | 0.54 |
ENT, Ear Nose and Throat; CI, confidence interval.

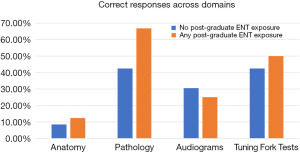
Respondents with any post-graduate ENT exposure were almost three-times more likely to correctly identify pathology on otoscopy (OR 2.7, 95% CI: 1.0–7.6; P=0.05) compared to those with no post-graduate experience. However, there was no significant difference in ability to correctly identify anatomy (OR 1.6, 95% CI: 0.3–7.2; P=0.59), interpret audiograms (OR 0.8, 95% CI: 0.2–2.2; P=0.64), and interpret tuning fork tests (OR 1.4, 95% CI: 0.5–3.6; P=0.54) (Table 4, Figure 3).
Table 4
| Ear examination domain | No post-graduate ENT experience | Any post-graduate ENT experience | Odds ratio (95% CI) (post-graduate ENT experience) | P value |
|---|---|---|---|---|
| Anatomy | 5/59 (8.5%) | 3/24 (12.5%) | 1.6 (0.3–7.2) | 0.59 |
| Pathology | 25/59 (42.4%) | 16/24 (66.7%) | 2.7 (1.0–7.6) | 0.05 |
| Audiograms | 18/59 (30.5%) | 6/24 (25%) | 0.8 (0.2–2.2) | 0.64 |
| Tuning Fork Tests | 25/59 (42.4%) | 12/24 (50%) | 1.4 (0.5–3.6) | 0.54 |
ENT, Ear Nose and Throat; CI, confidence interval.
When comparing interns to those with three or more years post-graduate years as a doctor, there was no significant difference between ability to correctly identify anatomy (P=0.88), pathology (P=0.75), audiograms (P=0.87) and tuning fork tests (P=0.26).
Discussion
This cross-sectional survey study demonstrated an overall lack of confidence in performing otoscopy and describing findings amongst junior doctors. There was no significant difference in ability to identify anatomy and pathology comparing doctors with no undergraduate ENT exposure to those with more than one week of ENT exposure. Post-graduate ENT experience was correlated with increased identification of pathology on otoscopy but no difference in identifying anatomy, interpreting tuning fork tests and interpreting audiograms.
This survey study has made some interesting findings that could generate debate on ENT education for medical students and junior doctors. Given the prevalence of ear-related pathology, an Australian Delphi-method study found that 92.6% of experts agreed that competence in otoscopy should be a mandatory skill for Australian medical graduates (3). However, our study results demonstrated that half of survey respondents could correctly identify otopathology and only one in ten could correctly identify anatomical landmarks on otoscopy. This is consistent with international literature from Ireland and the US with 50% of final-year medical students and junior doctors able to identify pathology on otoscopy correctly (4,5).
In our cohort, almost three-quarters of survey respondents had less than one week of ENT teaching during medical school and almost all the survey respondents felt that more ENT exposure during medical school or as a junior doctor would be useful. This reflects similar findings to a recent Australian survey of interns that found 88% had less than one week of ENT teaching during medical school and only one-third felt they had sufficient ENT exposure to prepare them for practice as a junior doctor (13). An ENT rotation during medical school is not feasible for every student, given the logistical constraints of teaching hospitals without ENT services and limited placements for the volume of medical students. However, structured didactic teaching on otoscopy has been associated with increased confidence in performing otoscopy and presents an alternative to an ENT rotation during medical school (4,6). With advancing technology, Australian medical schools could consider otoscopy simulation and virtual reality as teaching modalities as described in multiple studies (14-16). Structured otoscopy teaching should also be considered in the Health Education and Teaching Institute (HETI) mandatory intern education program.
There were several limitations that should be considered when interpreting the results of this study. Firstly, our response rate was only 10%, likely due to email distribution of the survey. Higher response rates may have been achieved by in-person distribution at intern teaching or several reminder emails to complete the survey. The sampling bias limits the external validity of the results as they make not be indicative of the wider cohort of junior doctors. Our data found no difference in ability to correctly identify all the domains of an ear exam between interns and those with more than three years of post-graduate experience. However, our cohort did have an uneven distribution of experience levels, reflecting a possible source of selection bias.
Furthermore, there was no delineation between ENT exposure during medical school and structured otoscopy teaching. Previous studies have shown that junior doctors and medical students increase their confidence in performing otoscopy with structured teaching rather than unstructured exposure that is often the case in medical student placements (6,7). The self-reported amount of ENT exposure during medical school represents possible recall bias and was not corroborated with individual medical schools as this data was not collected. Finally, use of Likert scales and questionnaires present an intrinsic source of response bias and restricted choice.
Conclusions
This study demonstrated an overall lack in self-reported confidence and competence in otoscopy amongst junior doctors. There was an overall deficiency in ability to identify anatomical landmarks, otopathology and interpret tuning fork tests amongst survey respondents. Further education through structured tutorials, at undergraduate level, or incorporated into HETI-mandated intern teaching, should be considered to increase the confidence of junior doctors to perform otoscopy and ensure safe clinical competency in this essential skill, especially if further studies support these findings.
Acknowledgments
None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://www.theajo.com/article/view/10.21037/10.21037/ajo-24-37/rc
Data Sharing Statement: Available at https://www.theajo.com/article/view/10.21037/ajo-24-37/dss
Peer Review File: Available at https://www.theajo.com/article/view/10.21037/ajo-24-37/prf
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://www.theajo.com/article/view/10.21037/ajo-24-37/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) with implied consent from all individual participants. The project was reviewed by the Northern NSW Local Health District Research Office under a non-Human Research Ethics Committee (HREC) pathway for low-risk projects and was deemed to be consistent with the principles and values outlined in the National Statement on Ethical Conduct in Human Research (2007). As a low-risk survey project, exemption was granted from HREC approval, in line with NSW Health policy.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sorichetti BD, Pauwels J, Jacobs TB, et al. High frequency of otolaryngology/ENT encounters in Canadian primary care despite low medical undergraduate experiences. Can Med Educ J 2022;13:86-9. [PubMed]
- AIHW. Emergency Department Care 2022-2023 2023. Available online: https://www.aihw.gov.au/reports-data/myhospitals/sectors/emergency-department-care
- Green P, Edwards EJ, Tower M. Core procedural skills competencies and the maintenance of procedural skills for medical students: a Delphi study. BMC Med Educ 2022;22:259. [Crossref] [PubMed]
- Wauchope J, Garry S, Guinness F, et al. Improving otoscopy education and diagnostic accuracy: A prospective interventional study. Int J Pediatr Otorhinolaryngol 2022;162:111267. [Crossref] [PubMed]
- Niermeyer WL, Philips RHW, Essig GF Jr, et al. Diagnostic accuracy and confidence for otoscopy: Are medical students receiving sufficient training? Laryngoscope 2019;129:1891-7. [Crossref] [PubMed]
- You P, Chahine S, Husein M. Improving learning and confidence through small group, structured otoscopy teaching: a prospective interventional study. J Otolaryngol Head Neck Surg 2017;46:68. [Crossref] [PubMed]
- Wormald PJ, Browning GG, Robinson K. Is otoscopy reliable? A structured teaching method to improve otoscopic accuracy in trainees. Clin Otolaryngol Allied Sci 1995;20:63-7. [Crossref] [PubMed]
- Inc. M. Survey Monkey San Mateo, California, USA: Momentive Inc.; Available online: www.momentive.ai
- Isaacson G. Tympanostomy Tubes-A Visual Guide for the Young Otolaryngologist. Ear Nose Throat J 2020;99:8S-14S. [Crossref] [PubMed]
- Salmon MK, Brant J, Hohman MH, et al. Audiogram Interpretation. 2023 Mar 1. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024.
- Alshuaib WB, Al-Kandari JM, Hasan SM. Classification of Hearing Loss [Internet]. Update On Hearing Loss. InTech; 2015.
- Team R. R Studio. 1.3.1093 ed. Boston, MA: RStudio Team; 2020.
- Yau S, Wong M, Cervin A. A survey of Queensland medical education in otolaryngology. Aust J Otolaryngol 2021;4:20. [Crossref]
- Stepniak C, Wickens B, Husein M, et al. Blinded randomized controlled study of a web-based otoscopy simulator in undergraduate medical education. The Laryngoscope 2017;127:1306-11. [Crossref] [PubMed]
- Davies J, Djelic L, Campisi P, et al. Otoscopy simulation training in a classroom setting: a novel approach to teaching otoscopy to medical students. Laryngoscope 2014;124:2594-7. [Crossref] [PubMed]
- Fieux M, Zaouche S, Philouze P, et al. Low-fidelity otoscopy simulation and anatomy training: A randomized controlled trial. Eur Ann Otorhinolaryngol Head Neck Dis 2021;138:231-4. [Crossref] [PubMed]
Cite this article as: Schnitzler N, Fox R, Kong JHK. Ear examination skills: a cross-sectional survey study of Australian junior doctors. Aust J Otolaryngol 2024;7:42.



