
Non-traumatic diplopia as a rare complication following functional endoscopic sinus surgery—case report
Introduction
Functional endoscopic sinus surgery (FESS) is widely used as a minimally invasive, effective treatment for patients with medically recalcitrant chronic rhinosinusitis (CRS) (1). The close proximity of the paranasal sinuses to critical structures in the orbit including the extra-ocular muscles and optic nerve, renders them vulnerable to damage during sinus surgery.
Orbital trauma post-FESS is rare, but can result in serious morbidity. Ophthalmic complications of FESS range from localised haematomas, lacrimal duct injury, retro-orbital haemorrhage to optic nerve injuries (2). Acute diplopia after FESS is more likely to be secondary to direct trauma to the extraocular muscles, the trochlea or superior oblique tendon, or orbital soft tissues. Intraoperative hypoperfusion leading to a microvascular cranial nerve palsy is more likely to occur in the acute setting. Delayed onset diplopia has a wider differential including underlying strabismus pathology.
This case series describes two patients who had diplopia post FESS. One was due to a decompensating esotropia, while the other had a microvascular abducens nerve palsy in the absence of pre-existing microvascular risk factors. While a rare occurrence, it is important to highlight the diverse causes of postoperative diplopia, which are not limited to orbital or muscle trauma. Furthermore, the optimisation of cardiovascular risk factors preoperatively is a pertinent consideration in FESS where there may be periods of intraoperative hypotension to achieve an adequate surgical field and haemostasis. We present this article in accordance with the CARE reporting checklist (available at https://www.theajo.com/article/view/10.21037/ajo-23-57/rc).
Case presentation
This is a retrospective observational case series of 2 patients who underwent FESS for CRS. Retrospective analysis of medical records was performed to obtain clinical data including demographics, comorbidities, visual outcomes, imaging studies, course of disease, surgery, intraoperative vitals assessment, surgical outcomes and follow-up.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Case 1
A 71-year-old man with severe CRS, bilateral nasal polyposis and septal deviation underwent septoplasty and FESS (Figure 1).
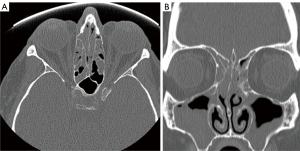
Case 1 had a history significant for hypertension and atrial fibrillation, which was treated with prazosin hydrochloride, olmesartan and lercanidipine. The patient, a retired primary care physician, had elected to self-discontinue his aspirin several months prior to his surgery. Preoperative arterial blood pressure was 120/82 mmHg. Anaesthesia was induced with propofol and his arterial blood pressure was decreased to 80/60 mmHg following induction and maintained at around 95/75 mmHg (blood pressure ranging between 80/60 and 118/72 mmHg). His mean arterial pressure (MAP) ranged between 66.7 and 87.3 mmHg intraoperatively, and was recorded below 75 mmHg for 15 minutes following propofol induction. The surgeon reported no intra-operative complications, and minimal blood loss. One month after undergoing FESS, the patient presented with diplopia. On examination, the patient had horizontal diplopia worse with mild limitation of left abduction. CT imaging did not demonstrate any signs of orbital trauma or sinus abnormalities (Figure 2). Magnetic resonance imaging (MRI) revealed moderate chronic small vessel ischaemia-related changes within the brain, with no abnormality detected along the pathway of the abducens nerve.

At 12 months’ follow-up, the patient reported intermittent diplopia due to decompensating esotropia. The ocular movements were full and this was confirmed on Hess chart, a chart used to assess extraocular movements and aid in the diagnosis of ocular motility defects. The patient reported intermittent diplopia, likely due to a decompensating esotropia (underlying strabismus). He was advised to use Fresnel prism glasses for symptomatic relief and was followed up with his general practitioner (GP) for optimisation of vascular risk factors. At last review with his ENT (ear, nose, and throat) surgeon, he reported very mild residual diplopia on far lateral gaze and had reported that he no longer needed to use his Fresnel prisms.
Case 2
A 71-year-old man with CRS, bilateral nasal polyposis and previous unsuccessful balloon sinuplasty 10 years prior underwent revision FESS (Figure 3).

His past medical history included asthma, benign prostatic hypertrophy and anxiety, and there was no history of cardiovascular disease. Preoperative arterial blood pressure was 140/82 mmHg. After the induction of anaesthesia, arterial blood pressure decreased to 110/60 mmHg. Throughout the surgery, the patient’s BP ranged from 78/50 to 105/60 mmHg. His MAP ranged from 59.33 to 75 mmHg, and was recorded below 75 mmHg for a duration of 135 minutes. There were no intraoperative complications. Ten days after undergoing FESS, he presented with visual blurring and diplopia. On examination, the patient had horizontal binocular diplopia on left lateral gaze with slow abducting saccades in the left eye. Cover test at distance demonstrated mild left esotropia in primary gaze for distance fixation target at 6 metres (single with 4 prism diopter base-out in all positions). There was mild limitation of abduction in the left eye and this was confirmed on Hess chart. No evidence of orbital or sinogenic pathology was identified on imaging to account for the diplopia (Figure 4). Given these findings, an isolated microvascular abducens nerve palsy was suspected. After 3 months, the patient reported that his diplopia had resolved. With no history of pre-operative vascular risk factors, this patient was also asked to follow up with his GP to assess and optimise these risk factors. On last review with his ENT surgeon 12 months following his procedure, he reported complete subjective resolution of his diplopia.

Discussion
FESS is an effective and relatively safe surgical procedure, with major complications including cerebrospinal fluid leak, meningitis, major haemorrhage and orbital trauma estimated to occur in less than 1% of cases (3). Diplopia is a rare complication that can develop after FESS. In this case series, we present 2 patients who developed delayed onset (subacute) diplopia 10–30 days after undergoing FESS to highlight alternative causes to the aforementioned factors.
In the acute postoperative period, diplopia may be caused by direct injury to an extra-ocular muscle or orbital soft tissue. The medial rectus muscle is the most common extra-ocular muscle to be inadvertently damaged during FESS, due to its close anatomic proximity to the thin lamina papyracea (4). The superior oblique tendon is also predisposed to injury during endoscopic frontal sinus drill-out and this can lead to Brown’s syndrome. Brown’s syndrome is a type of restrictive strabismus, characterized by limited elevation in adduction of the affected eye due to restriction of the superior oblique trochlea-tendon complex (5).
Most reported cases of diplopia after FESS are attributable to direct orbital trauma, with only a few publications describing the occurrence of post-FESS diplopia without proven orbital damage. Bayramlar et al. (6) reported a case of post-operative transient hypertropia, inferior oblique paresis, anisocoria and accommodation palsy, after bilateral endoscopic medial maxillectomies and revision Caldwell-Luc procedures for CRS. With no orbital or intracranial abnormalities demonstrated on post-operative imaging, this presentation was thought to have occurred due to a traumatic partial palsy of the inferior division of the right cranial nerve (CN) III. This may have resulted from perineural oedema from surgical manipulation around the lamina papyracea. Carter et al. (7) described a patient with intermittent exotropia with right hypotropia after FESS. The patient had mild limitation of right adduction and elevation. MRI revealed right medial rectus enlargement which was thought to be due to inflammation and oedema induced by the adjacent sinus. Kosko et al. (8) reported a patient with anisocoria and diplopia post-revision FESS, which gradually improved and completely resolved after 2 months. A diagnosis of a partial left oculomotor nerve palsy with parasympathetic deficiency due to perineural oedema was made, given there was normal orbital imaging.
Acute diplopia may also arise from hypoperfusion leading to a microvascular nerve palsy. A subacute presentation may be a coincidental occurrence in established vasculopathy. This emphasises the need for preoperative optimisation of cardiovascular risk factors and continuous intraoperative monitoring of MAP. During FESS, under general anaesthesia, an anaesthetic agent such as propofol is used to induce intraoperative hypotension (9). Deliberate controlled hypotension with reduction of MAP to 60–70 mmHg and systolic blood pressure to 80–90 mmHg in otherwise healthy patients is safe during FESS (10). Maintaining the intraoperative MAP within this range has also been shown to improve the surgical field and reduce intraoperative blood loss (11,12). In otherwise healthy patients undergoing FESS with general anaesthesia, reducing MAP to below 60 mmHg has been shown to reduce intracerebral perfusion and may increase the risk of cerebral ischemia. In rare cases, intraoperative hypotension can lead to ischemia of the cranial nerves (13). Paresis of the third, fourth and sixth cranial nerves are the most frequent, with patients generally presenting with ophthalmoplegia and visual disturbances (14). Hence, it is important in each FESS case to carefully evaluate the patient’s suitability for controlled hypotensive anaesthesia and optimise vascular risk factors pre-operatively (15). Vigilant monitoring of the intraoperative blood pressure readings should also be performed.
The mechanisms of subacute diplopia post-FESS in this case series were secondary to an underlying strabismus in Case 1 and microvascular abducens nerve palsy in Case 2. The patient described in Case 1 had a history of atrial fibrillation and hypertension, with moderate chronic small vessel ischaemia-related changes detected on MRI. As the patient in Case 1 was a known vasculopath, his pre-existing microvascular risk factors may have also contributed to the development of his diplopia. The timing of onset of diplopia was 1 month, so it was likely coincidental and the pattern of his ocular motility suggested a decompensating esotropia. An esophoria is a condition where the eyes have a tendency to deviate inwards but is overcome by maintenance of fusion; a decompensated esotropia occurs when there is a breakdown of fusion resulting in a constant deviation of the eye turning inwards. There was no established cardiovascular history in Case 2, but his spontaneous resolution after 3 months is consistent with a microvascular cranial nerve palsy which may have been precipitated by intraoperative hypotension.
The treatment of diplopia is dependent on the cause. Case 1 with underlying strabismus, was managed with prism glasses long-term. Meanwhile, Case 2 had a microvascular abducens nerve palsy which resolved spontaneously. The treatment of microvascular cranial nerve palsies consists of simple observation and most patients recover within 3–6 months.
Conclusions
In conclusion, diplopia is a rare but significant complication after FESS. This case series highlights 2 different causes of diplopia that occurred following FESS in the absence of intraoperative complications and no orbital trauma. The aetiology of diplopia in our case patients was underlying strabismus, and a microvascular cranial nerve palsy. In patients with high-risk cardiovascular histories undergoing FESS, the optimisation of cardiovascular risk factors and strict monitoring of intraoperative blood pressure are crucial in minimizing the risk of complications.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://www.theajo.com/article/view/10.21037/10.21037/ajo-23-57/rc
Peer Review File: Available at https://www.theajo.com/article/view/10.21037/ajo-23-57/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://www.theajo.com/article/view/10.21037/ajo-23-57/coif). A.J.P. serves as an unpaid editorial board member of Australian Journal of Otolaryngology from January 2019 to December 2024. A.J.P. has received grants from the NHMRC and Rodney Williams Memorial Foundation within the past 36 months. A.J.P. has received consulting fees for Medtronic and speakers hononaria for GSK, Storz, Medtronic and Sanofi. A.J.P. has received support for flights to conference from Storz and Medtronic. A.J.P. has an unpaid leadership role in ANZRS and ASOHNS. A.J.P. is a shareholder in Chitogel. A.J.P. has received sponsorship of FESS course from Storz, Medtronic, GSK, Sanofi, Stryker and ENT technologies. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- McMains KC. Safety in endoscopic sinus surgery. Curr Opin Otolaryngol Head Neck Surg 2008;16:247-51. [Crossref] [PubMed]
- Bhatti MT, Giannoni CM, Raynor E, et al. Ocular motility complications after endoscopic sinus surgery with powered cutting instruments. Otolaryngol Head Neck Surg 2001;125:501-9. [PubMed]
- Hosemann W, Draf C. Danger points, complications and medico-legal aspects in endoscopic sinus surgery. GMS Curr Top Otorhinolaryngol Head Neck Surg 2013;12:Doc06. [PubMed]
- Han JK, Higgins TS. Management of orbital complications in endoscopic sinus surgery. Curr Opin Otolaryngol Head Neck Surg 2010;18:32-6. [Crossref] [PubMed]
- Koc AA, Aygit ED, Inal A, et al. Brown Syndrome: Features and Long-term Results of Management. Beyoglu Eye J 2021;6:223-8. [PubMed]
- Bayramlar H, Miman MC, Demirel S. Inferior oblique paresis, mydriasis, and accommodative palsy as temporary complications of sinus surgery. J Neuroophthalmol 2004;24:225-7. [Crossref] [PubMed]
- Carter K, Lee AG, Tang RA, et al. Neuro-ophthalmologic complications of sinus surgery. Neuro-Ophthalmology 1998;19:75-82. [Crossref]
- Kosko JR, Pratt MF, Chames M, et al. Anisocoria: a rare consequence of endoscopic sinus surgery. Otolaryngol Head Neck Surg 1998;118:242-4. [Crossref] [PubMed]
- Boonmak P, Boonmak S, Laopaiboon M. Deliberate hypotension with propofol under anaesthesia for functional endoscopic sinus surgery (FESS). Cochrane Database Syst Rev 2016;10:CD006623. [Crossref] [PubMed]
- Kwon Y, Jang JS, Hwang SM, et al. Range of S-100β levels during functional endoscopic sinus surgery with moderately controlled hypotension. Eur Arch Otorhinolaryngol 2017;274:3527-32. [Crossref] [PubMed]
- Zhao YC, Psaltis AJ. Hemostasis in sinus surgery. Curr Opin Otolaryngol Head Neck Surg 2016;24:26-30. [Crossref] [PubMed]
- Sia DI, Chalmers A, Singh V, et al. General anaesthetic considerations for haemostasis in orbital surgery. Orbit 2014;33:5-12. [Crossref] [PubMed]
- Ha TN, van Renen RG, Ludbrook GL, et al. The relationship between hypotension, cerebral flow, and the surgical field during endoscopic sinus surgery. Laryngoscope 2014;124:2224-30. [Crossref] [PubMed]
- Savoiardo M, Minati L, Farina L, et al. Spontaneous intracranial hypotension with deep brain swelling. Brain 2007;130:1884-93. [Crossref] [PubMed]
- Saxena A, Nekhendzy V. Anesthetic considerations for functional endoscopic sinus surgery: a narrative review. Journal of Head and Neck Anesthesia 2020;4:e25. [Crossref]
Cite this article as: Lam L, Tong JY, Simon S, Selva D, Psaltis AJ. Non-traumatic diplopia as a rare complication following functional endoscopic sinus surgery—case report. Aust J Otolaryngol 2024;7:24.


