
Examination of burnout for severity and risk factors in New Zealand otolaryngologists: a cross-sectional study
Introduction
Burnout is an important phenomenon amongst healthcare professionals (1). The 11th Revision of the International Classification of Diseases (ICD-11) describes burnout as an occupational syndrome resulting from chronic work-related stress (2), characterised by a triad of emotional exhaustion (EE), depersonalisation (DP), and reduced personal accomplishment (PA) (3).
Identifying burnout amongst medical specialists can help protect our workforce and maintain our safe health system. As with other medical and surgical specialities, burnout is increasing within the specialty of otolaryngology (ORL) (4,5).
There are multiple demands on ORL surgeons including clinical workload, technically demanding surgeries, high patient and professional expectations, the emotional distress of patient morbidity and mortality, time pressures, interpersonal conflicts, and departmental burdens (4,6). Personal characteristics of self-criticism, perfectionism, and a suboptimal social support system are also associated with burnout (1). Burnout is associated with poor job satisfaction and reduced productivity. Medical errors are more likely to occur due to burnout, and therefore safe patient care is compromised (1,6,7). Earlier retirement due to burnout results in a loss of resource-intensive training and necessitates employing a replacement (1). In addition to these professional implications, there are numerous personal implications such as higher complaints of exhaustion, fatigue, stress, depression, substance abuse, and impact on personal relationships and family (1,6,8). Several studies have recognised that many of these contributory factors are modifiable, so early identification and intervention can help prevent burnout and its consequences (4,6).
This study sought to identify burnout amongst consultant ORL surgeons in New Zealand. Due to the relatively small number of ORL surgeons operating within the country, even a modest reduction in the workforce can profoundly impact the delivery of ORL care on a national level. In this study, the survey instrument used was the Maslach Burnout Inventory - Human Services Study (MBI-HSS), a robust tool in assessing this occupational syndrome (3,4). The questionnaire consists of 22 questions to measure three dimensions of burnout: EE, DP, and PA. We present this article in accordance with the STROBE reporting checklist (available at https://www.theajo.com/article/view/10.21037/ajo-23-24/rc).
Methods
Participants
This study was a cross-sectional, questionnaire-based examination of consultant ORL, Head and Neck surgeons (ORL-HNS) in New Zealand. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Informed consent was taken from all individual participants. The Northland District Health Board locality assessment committee (Locality assessment number 2020-06) provided ethical approval, and the New Zealand Health and Disability Ethics Committee (HDEC) provided an out-of-scope letter. Surgeon details were retrieved from the New Zealand Society of Otolaryngology-Head and Neck Surgery (NZSOHNS) register, Healthpoint (an online register of health professionals in New Zealand) and each of the 20 individual District Health Board (DHB) websites. All surgeons with Fellowship of the Royal Australasian College of Surgeons in Otolaryngology (or international equivalent) were included in the study. There were no exclusion criteria. As New Zealand is a relatively small country with a small ORL-HNS workforce, a practical decision was made to include all New Zealand consultant ORL-HNS in the sample group to maximise the statistical power. Raftopulos et al. utilised similar logic when examining burnout amongst the specific, relatively small population of ORL-HNS trainees in Australia (9). Anonymised, paper-based questionnaires were sent via courier in March 2020 to each surgeon. A separate consent form was enclosed with two postage-paid return envelopes. For those that did not send a paper response (based on returned consent forms), questionnaires were sent via email using an online survey platform (SurveyMonkey) to improve the response rate. All survey responses were kept confidential and processed anonymously by the lead author (C.B.P.). Survey responses were collected over a 6-month period due to delayed responses in the global severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [coronavirus disease-2019 (COVID-19)] pandemic environment. Non-duplication of responses was ensured by the SurveyMonkey platform, which only allowed one response for each unique email address.
Burnout survey
All participants answered 22 questions across the three domains of burnout in the MBI-HSS instrument: EE, DP and low PA. There are 9, 5 and 8 questions within each domain, respectively. Each question was answered on a 7-point Likert scale from “Never” (0) to “Every day” (6). The severity of burnout in each domain was categorised based on predefined scores (9,10).
EE scores of <17, 17–26, and >26 and DP scores of <9, 9–13, and >13 were classified as low, moderate, and high respectively. Because of PA’s inverse relationship with burnout, scores of >36, 31–36, and <31 were respectively classified as low, moderate, and high risk. In concordance with multiple other studies, categorical burnout was defined as having a high score in any one of the three domains (9). An individual’s risk of burnout was categorised as:
- Low if the scores in all three domains were low;
- Moderate if at least one domain had a moderate score;
- High if at least one domain had a high score;
- Severe if more than one domain had a high score.
Risk factors and correlations
In addition to the MBI-HSS, respondents also completed another questionnaire developed by the authors that assessed potential correlating risk factors (included in Appendix 1). The questions were divided into demographic and professional factors, with 8 and 14 questions in each category. The demographic questions examined gender, age, ethnicity, partner status, children status and practice urbanicity. The professional category examined subspeciality of practice, public and private work split, years spent as a senior medical officer (SMO), average weekly work hours, weekend work, and the impacts work had on personal, social, and family life.
Statistical analysis
Univariate statistical analysis was conducted on each potential risk factor to identify the degree of correlation with burnout. The degree of correlation between categorical variables was assessed using a chi-square test. Kendall’s tau-B test was performed on ordinal variables. The correlation was categorised as strong if Kendall’s tau-B coefficient was >0.5, moderate if it was 0.2–0.5, and weak if <0.2 (9). Of participants that completed the surveys, the responses were almost entirely complete. One individual chose not to answer the question “Do you feel that you are suffering from burnout?”—this response was therefore omitted from correlation analysis for that specific question.
In addition to assessing correlation with burnout as defined by the MBI-HSS, correlation with the raw sum score of the three MBI domains was also assessed.
This was the sum of the EE and DP scores and the inverse PA score. PA has an inverse relationship with burnout, meaning that a low score confers a high burnout risk, and a high score is protective against burnout, which has been demonstrated by multiple previous studies (11,12). Therefore, the inverse PA score was used for the raw score, this was calculated by subtracting the total PA score from 48 (maximum possible PA score).
Correlation between the raw score and each ordinal variable was assessed using Kendall’s tau-B test. Two-sided P value tests were used, statistical significance was defined as a P value less than 0.05. All statistical analysis was performed on IBM SPSS Statistics Subscription Version 1.0.0.1461 (IBM, Armonk, New York, USA).
Results
Questionnaires were sent to 109 ORL-HNS in New Zealand, with a complete response rate of 68.8% (n=75). All 75 complete responses were analysed. 18.7% of respondents were female (n=14). 13.3% of respondents were younger than 40 years of age (n=10), 21.3% were 40–50 years of age (n=16), 33.3% were 50–60 years of age (n=25), 29.3% were 60–70 years of age (n=22) and 2.7% were greater than 70 years of age (n=2). The prevalence of burnout amongst respondents was 37.3% (n=28). These individuals had a high risk of burnout in at least one of the three MBI-HSS domains. Of all respondents, 9.3% (n=7) were severely burnt out, 28% (n=21) had high risk of burnout, 25.3% (n=19) had moderate risk and 37.3% (n=28) had low risk.
Correlation between demographic factors and burnout
There was no statistically significant correlation between demographic variables and burnout as defined by the MBI-HSS (having at least one category score high). The correlation between these demographic factors and the raw score (defined in the Methods section above) was assessed. A moderately strong and statistically significant inverse correlation was found with age [rt=0.230, 95% confidence interval (CI): 0.080–0.369, P=0.009], younger respondents tended to have a higher raw score. Of the respondents who met the MBI-HSS definition of burnout, 17.9% (n=5) were under the age of 40 years, 21.4% (n=6) were aged 40 to 50 years, and 42.9% (n=12) were aged 50 to 60 years. In total, 82.2% of burnt-out respondents were under the age of 60 years while only 59.6% of not burntout respondents were under the age of 60 years.
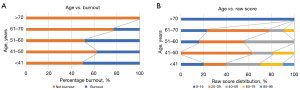
Figure 1 demonstrates how the raw score provides a clearer demonstration of correlation between age and burnout risk compared with using burnout as defined by MBI-HSS alone.
No statistically significant correlation was found between burnout and the number of dependent children (rt=0.148, 95% CI: −0.005 to 0.295, P=0.168). There was, however, a weak but statistically significant correlation between the raw score and the number of dependent children (rt=0.197, 95% CI: 0.045–0.340, P=0.02). These results are summarised in Table 1.
Table 1
| Demographic factors | Respondents, % | P value | Statistical test | Correlation coefficient (95% confidence interval) | |
|---|---|---|---|---|---|
| Burnt out | Not burnt out | ||||
| Respondents, n (%) | 28 (37.3) | 47 (62.7) | |||
| Gender | |||||
| Female | 28.6 | 13.0 | |||
| Male | 71.4 | 87.0 | 0.09 | Chi-square | |
| Age (years) | |||||
| <41 | 17.9 | 10.6 | |||
| 41–50 | 21.4 | 21.3 | |||
| 51–60 | 42.9 | 27.7 | |||
| 61–70 | 17.9 | 36.2 | 0.09 | Kendall’s tau-B (Burnt-out) | 0.175 (0.023–0.319) |
| >70 | 0 | 4.3 | 0.009* | Kendall’s tau-B (EE + DP + PA) | 0.230 (0.080–0.369) |
| Partners | |||||
| Have a partner/spouse | 100.0 | 95.7 | |||
| Healthcare professional partner/spouse | 57.1 | 61.7 | 0.53 | ||
| Number of dependents | |||||
| 0 | 25.0 | 41.3 | |||
| 1 | 28.6 | 23.9 | |||
| 2 | 32.1 | 26.1 | |||
| 3 | 10.7 | 6.5 | 0.16 | Kendall’s tau-B (Burnt-out) | 0.148 (−0.005–0.295) |
| 4 | 3.6 | 2.2 | 0.02* | Kendall’s tau-B (EE + DP + PA) | 0.197 (0.045–0.340) |
| Practice location | |||||
| Urban practice | 64.3 | 74.5 | |||
| Regional practice | 35.7 | 25.5 | 0.34 | Chi-square | |
*, P≤0.05. EE, emotional exhaustion; DP, depersonalisation; PA, personal accomplishment.
Correlation between professional/work-related factors and burnout
A strong and statistically significant correlation was found between the sense of feeling burdened by on-call demands and burnout [χ2(1, n=75)=13.385, P<0.001]. 60.7% (n=17) of burnt-out respondents indicated that they felt burdened by on-call demands. Only 19.1% (n=9) of not burnt-out respondents shared that feeling.
A moderate correlation was also found between the degree of general career dissatisfaction and burnout (rt=0.423, 95% CI: 0.289–0.540, P<0.001). Of the respondents not burnt out, 89.4% (n=42) either agreed or strongly agreed that they were satisfied with their career. Only 46.4% (n=13) of the burnt-out group agreed or strongly agreed with this.
There was a moderately strong correlation between burnout and the frequency of missing social activities due to work (rt=0.361, 95% CI: 0.221–0.487, P<0.001). A similar correlation was seen with the frequency of completing work-related tasks beyond work hours (rt=0.208, 95% CI: 0.057–0.350, P=0.04).
No statistically significant correlation was found between the number of years a respondent had worked as a consultant and burnout [rt=0.079, 95% CI: −0.075 to 0.229, P=0.45). There was also no statistically significant association with subspecialty of practice (P>0.05 for each individual subspeciality), public-private work split [χ2(2, n=75)=2.321, P=0.31], work hours per week [rt=0.101, 95% CI: −0.052 to 0.250, P=0.34), support from peers [χ2(1, n=74)=0.083, P=0.77], and support from organisations such as Medical Protection Society (MPS) [χ2(1, n=75)=1.095, P=0.295]. These results are summarised in Table 2.
Table 2
| Professional factors | Respondents, % [n] | P value | Statistical test | Correlation coefficient (95% confidence interval) | |
|---|---|---|---|---|---|
| Burnt out (n=28) | Not burnt out (n=47) | ||||
| Feeling burnt out | 50 [14] | 6.5 [3] | <0.001* | Chi-square | |
| Feeling burdened by on-call demands | 60.7 [17] | 19.1 [9] | <0.001* | Chi-square | |
| Sense of job dissatisfaction (I am satisfied with my career) | |||||
| Strongly disagree | 3.6 [1] | 2.1 [1] | |||
| Disagree | 14.3 [4] | 2.1 [1] | |||
| Neutral | 35.7 [10] | 6.4 [3] | |||
| Agree | 39.3 [11] | 59.6 [28] | <0.001* | Kendall’s tau-B (Burnt-out) | 0.423 (0.289–0.540) |
| Strongly agree | 7.1 [2] | 29.8 [14] | <0.001* | Kendall’s tau-B (EE + DP + PA) | 0.386 (0.248–0.509) |
| Frequently missing social activities | |||||
| Everyday | 3.6 [1] | 0 [0] | |||
| A few times per week | 14.3 [4] | 4.3 [2] | |||
| Once per week | 10.7 [3] | 4.3 [2] | |||
| A few times per month | 39.3 [11] | 21.3 [10] | |||
| Once per month | 7.1 [2] | 4.3 [2] | |||
| A few times per year | 21.4 [6] | 59.6 [28] | <0.001* | Kendall’s tau-B (Burnt-out) | 0.361 (0.221–0.487) |
| Never | 3.6 [1] | 6.4 [3] | <0.001* | Kendall’s tau-B (EE + DP + PA) | 0.320 (0.176–0.450) |
| Completing work tasks beyond work hours | |||||
| Everyday | 28.6 [8] | 23.4 [11] | |||
| A few times per week | 57.1 [16] | 31.9 [15] | |||
| Once per week | 0 [0] | 12.8 [6] | |||
| A few times per month | 10.7 [3] | 10.6 [5] | |||
| Once per month | 0 [0] | 6.4 [3] | |||
| A few times per year | 3.6 [1] | 10.6 [5] | 0.04* | Kendall’s tau-B (Burnt-out) | 0.208 (0.057–0.350) |
| Never | 0 [0] | 4.3 [2] | 0.004* | Kendall’s tau-B (EE + DP + PA) | 0.252 (0.103–0.389) |
| Checking work items beyond work hours | |||||
| Everyday | 57.1 [16] | 48.9 [23] | |||
| A few times per week | 28.6 [8] | 31.9 [15] | |||
| Once per week | 3.6 [1] | 2.1 [1] | |||
| A few times per month | 0 [0] | 10.6 [5] | |||
| Once per month | 3.6 [1] | 0 [0] | |||
| A few times per year | 7.1 [2] | 6.4 [3] | 0.49 | Kendall’s tau-B (Burnt-out) | 0.074 (−0.079–0.224) |
| Never | 0 [0] | 0 [0] | 0.07 | Kendall’s tau-B (EE + DP + PA) | 0.160 (0.008–0.305) |
| Number of years as an SMO | |||||
| <5 | 10.7 [3] | 8.5 [4] | |||
| 5–10 | 14.3 [4] | 19.1 [9] | |||
| 11–20 | 42.9 [12] | 23.4 [11] | |||
| 21–30 | 17.9 [5] | 31.9 [15] | 0.45 | Kendall’s tau-B (Burnt-out) | 0.079 (−0.075–0.229) |
| >30 | 14.3 [4] | 17.0 [8] | 0.03* | Kendall’s tau-B (EE + DP + PA) | 0.180 (0.028–0.323) |
| Subspecialities of practice† | |||||
| General | 57.1 [16] | 51.1 [24] | 0.61 | Chi-square | |
| Head and neck | 21.4 [6] | 29.8 [14] | 0.42 | Chi-square | |
| Sleep surgery | 10.7 [3] | 10.6 [5] | 0.99 | Chi-square | |
| Rhinology | 50.0 [14] | 42.6 [20] | 0.53 | Chi-square | |
| Otology | 32.1 [9] | 25.5 [12] | 0.53 | Chi-square | |
| Laryngology | 10.7 [3] | 8.5 [4] | 0.75 | Chi-square | |
| Paediatric | 32.1 [9] | 14.9 [7] | 0.07 | Chi-square | |
| Facial plastics | 7.1 [2] | 17.0 [8] | 0.22 | Chi-square | |
| Public–private split | |||||
| Public only | 14.3 [4] | 25.5 [12] | |||
| Private only | 3.6 [1] | 8.5 [4] | |||
| Public and private | 82.1 [23] | 66.0 [31] | 0.31 | Chi-square | |
| Hours of work per week | |||||
| <40 | 10.7 [3] | 19.1 [9] | |||
| 41–50 | 57.1 [16] | 31.9 [15] | |||
| 51–60 | 28.6 [8] | 34.0 [16] | |||
| 61–70 | 3.6 [1] | 14.9 [7] | 0.34 | Kendall’s tau-B (Burnt-out) | 0.101 (−0.052–0.250) |
| >70 | 0.0 [0] | 0.0 [0] | 0.57 | Kendall’s tau-B (EE + DP + PA) | 0.050 (−0.103–0.201) |
| Support | |||||
| Feel supported by peers | 89.3 [25] | 89.4 [42] | 0.77 | Chi-square | |
| Feel supported by organisations (i.e., MPS) | 67.9 [19] | 78.7 [37] | 0.29 | Chi-square | |
†, respondents were able to select multiple subspecialities of practice. *, P≤0.05. EE, emotional exhaustion; DP, depersonalisation; PA, personal accomplishment; SMO, senior medical officer; MPS, Medical Protection Society.
Predictive accuracy of ORL-HNS identifying personal burnout
When asked if they felt burnt out, the accuracy of an ORL-HNS surgeon’s response was assessed by comparing it with their true burnout status (based on the result of their response to the MBI-HSS). In this study, the sensitivity of this single question in identifying burnout was only 50%; however, the specificity was 93.5%. This response’s positive and negative predictive values were 82.4% and 75.4%, respectively. Additionally, of the 9% (n=7) of respondents identified as suffering severe burnout, 57.1% (n=4) identified that they felt burnt out, while 42.9% (n=3) did not, χ2(1, n=74)=18.594, P<0.001. These results are summarised in Table 3.
Table 3
| Feel burnt out | Truly burnt out† | ||
|---|---|---|---|
| Yes | No | Total | |
| Yes | 14 | 3 | 17 |
| No | 14 | 43 | 57 |
| Total | 28 | 46a | |
†, as defined by the MBI-HSS. a, one respondent who was not burnt out (as defined by the MBI-HSS) chose not to respond to this question. MBI-HSS, Maslach Burnout Inventory - Human Services Survey.
Discussion
This study showed a significant prevalence (37.3%) of burnout amongst consultant Otolaryngologists in New Zealand. Several factors were identified as having a statistically significant correlation with likelihood of burnout, these include feeling burdened by on-call demands, sense of job dissatisfaction, frequently missing social activities, completing work tasks beyond work hours and subjectively feeling burnt out.
There was a statistically significant correlation between ORL consultants feeling burnt out and meeting the MBI-HSS definition, suggesting that they were able to accurately identify their own burnout. It was reassuring to see the accuracy of that particular question as a very simple screening tool. With a specificity of 93.5%, it is reasonable to conclude that respondents answering “yes” to the question—Do you feel you are suffering from burnout?—were highly likely to be experiencing burnout. However, the false-negative rate was 50% (14/28), suggesting that a “no” response to that question should not have excluded burnout.
Multiple previous studies have been completed in exclusive cohorts of ORL-HNS and have attempted to identify correlating risk factors. A study in 2011 by Fletcher et al. (4) examined burnout amongst 115 ORL-HNS respondents and found younger age and fewer years in ORL practice as statistically significant risk factors, as did other previous studies (13,14). A study of 186 ORL-HNS by Carlson et al. found in a univariable setting that age, weekly hours worked, weekly nights on call and years of practice were all significantly correlated with distress (15).
Career dissatisfaction was a strong predictor of burnout in this study, with a Kendall’s tau-B value of 0.423, demonstrating a moderate strength of correlation (P<0.001). The difficulty with interpreting this result was in trying to evaluate causation—it seemed plausible that a higher degree of burnout would result in greater overall career dissatisfaction, but it also equally seemed plausible that reduced overall career satisfaction led to increasing burnout. The authors of this study felt that the reality was likely to be somewhere in the middle, with both factors having a complex relationship. In either case, it seemed reasonable to infer that an ORL consultant expressing reduced career satisfaction was likely also suffering burnout.
In concordance with other previous studies, burnout had a statistically significant, moderate inverse correlation with age and a weak (but statistically significant) association with years worked as an SMO (4,13-15). This correlation was only found when the raw score was compared with those factors (Kendall’s tau-B test).
While there have been varying results in previous studies assessing the correlation between hours worked per average week and burnout, this study did not reveal any statistically significant correlation.
In this study, the sample size was smaller than other previous similar studies, which included participant numbers in the hundreds or even thousands. Furthermore, using a dichotomous measure of burnout (as defined by the MBI-HSS) to evaluate for correlation with potential risk factors could have missed possibly important correlations, whereas using the raw score increased the sensitivity of finding such correlations. This was expected by the authors, as it is well understood that mental health disorders lie on a continuous spectrum rather than a dichotomous disease state such as cancer.
This study established a raw score by taking the sum of the EE and DP scores and the inverse PA score. In this study, a statistically significant correlation between age and burnout was not found. However, a statistically significant inverse correlation between age and the raw score was found, and this was concordant with other studies that have assessed for age. Figure 1 demonstrates this difference. The authors felt that this supports the validity of using the raw score (as defined in the methods section) to identify risk factors that may otherwise not correlate with categorical burnout in a statistically significant way. Some studies have elected to give PA less attention as there has been some evidence that EE and DP scores have a strong correlation with burnout independent of the PA score (4,16). The authors of this study felt that it was more valid to include the PA score than to ignore it.
In this study, the respondents were categorised into low, moderate, and high burnout risk, as well as severe burnout. This made logical sense to the authors as it is well understood that mental health disorders lie on a continuous spectrum (17) and previous studies have devised similar categories (4,18).
Limitations of this study include relatively small sample size and the long timeframe of 6 months to collect all survey responses. The global COVID-19 pandemic certainly affected response rates and potentially also contributed to increased burnout. Despite these limitations, the results are similar to that of other previous studies with a high prevalence of nearly two in five surgeons demonstrating burnout.
Conclusions
This study was the first to exclusively examine burnout amongst the entire ORL consultant workforce in New Zealand. It identified a 37.3% rate of burnout.
The strongest correlating risk factors in this study were respondents feeling burnt-out, feeling burdened by on-call demands, overall career dissatisfaction, frequently missing social activities and completing work-related tasks beyond work hours. This study highlighted the high prevalence of burnout, a serious mental health concern, amongst a vital component of New Zealand’s healthcare workforce.
Addressing burdensome on-call demands, achieving work-life balance, and preventing work from encroaching on important social activities are likely to have a positive impact on burnout. These changes may occur at departmental, organisational, or national levels.
The authors suspect there is a significant prevalence of burnout amongst other groups of healthcare professionals who also experience many of the same potential risk factors. There is a broad scope for future research in this area that could include examining burnout amongst the wider national surgical and physician workforce, junior doctor workforce, and nursing/allied health workforce. Qualitative, interview-based research is also likely to yield important information in this area.
Acknowledgments
The manuscript was presented at New Zealand Society of Otolaryngology, Head and Neck Surgery 73rd Annual General and Scientific Meeting in 2020.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://www.theajo.com/article/view/10.21037/ajo-23-24/rc
Data Sharing Statement: Available at https://www.theajo.com/article/view/10.21037/ajo-23-24/dss
Peer Review File: Available at https://www.theajo.com/article/view/10.21037/ajo-23-24/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://www.theajo.com/article/view/10.21037/ajo-23-24/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately in-vestigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The Northland District Health Board locality assessment committee (Locality assessment number 2020-06) provided ethical approval. Informed consent was taken from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Patel RS, Bachu R, Adikey A, et al. Factors Related to Physician Burnout and Its Consequences: A Review. Behav Sci (Basel) 2018;8:98. [Crossref] [PubMed]
- QD85 Burnout. World health Organization. World Health Organization; 2021 [cited 2021Aug15]. Available online: https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/129180281
- Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol 2001;52:397-422. [Crossref] [PubMed]
- Fletcher AM, Pagedar N, Smith RJ. Factors correlating with burnout in practicing otolaryngologists. Otolaryngol Head Neck Surg 2012;146:234-9. [Crossref] [PubMed]
- Geelan-Hansen K, Anne S, Benninger MS. Burnout in Otolaryngology-Head and Neck Surgery: A Single Academic Center Experience. Otolaryngol Head Neck Surg 2018;159:254-7. [Crossref] [PubMed]
- Lawlor SK, Low CM, Carlson ML, et al. Burnout and well-being in otolaryngology trainees: A systematic review. World J Otorhinolaryngol Head Neck Surg 2022;8:118-25. [Crossref] [PubMed]
- Al-Ghunaim TA, Johnson J, Biyani CS, et al. Surgeon burnout, impact on patient safety and professionalism: A systematic review and meta-analysis. Am J Surg 2022;224:228-38. [Crossref] [PubMed]
- Vijendren A, Yung M, Shiralkar U. Are ENT surgeons in the UK at risk of stress, psychological morbidities and burnout? A national questionnaire survey. Surgeon 2018;16:12-9. [Crossref] [PubMed]
- Raftopulos M, Wong EH, Stewart TE, et al. Occupational Burnout among Otolaryngology-Head and Neck Surgery Trainees in Australia. Otolaryngol Head Neck Surg 2019;160:472-9. [Crossref] [PubMed]
- Byrne BM. Testing for the Factorial Validity, Replication, and Invariance of a Measuring Instrument: A Paradigmatic Application Based on the Maslach Burnout Inventory. Multivariate Behav Res 1994;29:289-311. [Crossref] [PubMed]
- Balch CM, Shanafelt TD, Sloan J, et al. Burnout and career satisfaction among surgical oncologists compared with other surgical specialties. Ann Surg Oncol 2011;18:16-25. [Crossref] [PubMed]
- West CP, Dyrbye LN, Sloan JA, et al. Single item measures of emotional exhaustion and depersonalization are useful for assessing burnout in medical professionals. J Gen Intern Med 2009;24:1318-21. [Crossref] [PubMed]
- Golub JS, Johns MM, Weiss PS, et al. Burnout in Academic Faculty of Otolaryngol-ogy-Head and Neck Surgery. Laryngoscope 2008;118:1951-6. [Crossref] [PubMed]
- Dyrbye LN. Relationship between work-home conflicts and burnout among American surgeons. Arch Surg 2011;146:211. [Crossref] [PubMed]
- Carlson ML, Larson DP, O'Brien EK, et al. Prevalence of and Associations With Distress and Professional Burnout Among Otolaryngologists: Part II, Attending Physicians. Otolaryngol Head Neck Surg 2021;164:1030-9. [Crossref] [PubMed]
- Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory. In: Zalaquett CP, Wood RJ. editors. Evaluating Stress: A Book of Resources. Lanham, MD: The Scarecrow Press; 1997.
- Crocq MA. The history of generalized anxiety disorder as a diagnostic category. Dialogues Clin Neurosci 2017;19:107-16. [Crossref] [PubMed]
- Johns MM 3rd, Ossoff RH. Burnout in academic chairs of otolaryngology: head and neck surgery. Laryngoscope 2005;115:2056-61. [Crossref] [PubMed]
Cite this article as: Patel CB, Heaven C, Waterhouse D, Roberts M, Shetty S. Examination of burnout for severity and risk factors in New Zealand otolaryngologists: a cross-sectional study. Aust J Otolaryngol 2024;7:15.


