Functional and aesthetic outcomes of dermofat graft reconstruction in limited parotidectomy defects: a cross-sectional study
Introduction
The first-line treatment for benign parotid tumours is complete surgical excision with preservation of the facial nerve (1). Complications of parotid surgery include salivary leak and sialocoele, bleeding, infection, and Frey’s syndrome. Parotidectomy can leave patients with an unsightly facial hollowing especially when large portions of the gland are removed. Various reconstructive methods have been described to restore the natural contour of the face and create a barrier between the parotid bed and skin to help prevent Frey’s syndrome, including local flaps and tissue grafts (2-11). Each method has its benefits and disadvantages, and none have demonstrated clear superiority over the rest (12,13). One reconstructive method that has been described is using a dermofat graft from the abdomen which has appeal due to ease of donor site graft harvesting, ability to mould to the defect, and minimal donor site morbidity (12,14,15). Current publications on the complication rates and patient cosmetic satisfaction post-dermofat grafting are limited by their small and heterogeneous cohorts. This study aimed to assess the cosmetic satisfaction and complication rates associated with the use of dermofat graft reconstruction in limited parotidectomies for benign disease aetiologies. We present this article in accordance with the STROBE reporting checklist for cross-sectional studies (available at https://www.theajo.com/article/view/10.21037/ajo-23-30/rc).
Methods
Study design
A retrospective cross-sectional study using a self-developed questionnaire was generated. Patients were identified from the Sydney Head and Neck Cancer Institute Head & Neck Surgery Database. Inclusion criteria were patients aged over 18 years old who underwent limited parotidectomy with dermofat graft reconstruction for benign parotid tumours between 2013–2021 and consented to participate in the study. Exclusion criteria were patients under 18 years of age and all patients that had parotidectomy for cancer or for benign pathology that did not have a dermofat reconstruction. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the St Vincent’s Hospital Human Research Ethics Committee (2021/ETH11634) and informed consent was obtained from all participants.
Surgical technique
The standard ablative technique is used to remove the parotid tumour. The dermofat graft is either taken from (I) the groin or iliac region or (II) periumbilical region according to surgeon preference but factors such as the amount of fat tissue and scar location are taken into account. After the parotid tumour is excised, an assessment is made as to the volume of the defect. An elliptical incision is placed with the size of the incision and depth matching the defect in the parotid gland. The next step is to remove the overlying epidermis whilst leaving the underlying dermis intact. Care must be taken in this step to make sure that all the epidermis is removed. This can be readily achieved by using the cutting setting on a monopolar diathermy and traction. Once the epidermis is removed, the base of the dermofat graft is transected in a horizontal plane parallel to the overlying dermis. Haemostasis is obtained at the donor site and then the donor site is closed in 2 layers. A drain is not required in the donor site. The dermofat graft is then placed in the parotid defect and trimmed to match the defect (Figure 1). Slight overfilling of the height of the defect with the dermofat graft is advised as the dermofat graft will shrink around 20% (16). With the dermal edge most superficial, the dermofat graft is sutured into position with radial absorbable suture (such as Vicryl) with care taken to avoid any sutures near branches of the facial nerve. A small drain is placed away from the facial nerve and the overlying skin is then replaced over the parotid bed and the skin closed as per the surgeon’s preference. Wound closure strips (such as 3M Steri-Strips) are applied along the line of incision and routine antibiotics to cover skin organisms (cephalexin 500 mg three times daily for 7 days) are prescribed.

Population characteristics
Clinical records, operation reports and pathological reports were reviewed to gather demographic data (date of birth, gender, contact details), surgical details (surgery date and type, dermofat graft donor site) and pathological data (tumour histopathological type and size).
Post-operative complications
Information on post-operative complications from the donor site and parotid site, such as haematoma, infection, and seromas or sialocoeles, were gathered from the Sydney Head and Neck Cancer Institute Head & Neck Surgery Database and clinical records. Parotid seroma, salivary leaks, and sialocoeles were grouped together as “parotid sialocoeles” because it was not possible to distinguish between these retrospectively.
Patient-reported outcomes
A self-developed questionnaire was created and sent out to participants to obtain patient-reported outcomes on donor site issues (numbness, pain, and impact of scar), and issues relating to the parotid surgical site (gustatory sweating and cosmetic satisfaction). The patient experience of post-operative complications and concerns regarding the donor site scar was recorded on a four-point Likert scale from “not at all” to “severely” while the cosmetic appearance rating was recorded on a five-point scale of “very bad” to “very good”. These terms were not objectively defined, rather patients were allowed to describe a severity variable relevant to them. These were distributed alongside an invitation letter and patient information sheet via email through the REDCap survey distribution system or post. If no response was obtained after three weeks, one contact attempt was made by phone to obtain verbal consent and questionnaire responses.
Statistical analysis
Descriptive statistics and frequency calculations were completed on IBM SPSS Statistics for Macintosh, version 26.0 (IBM Corp., New York, USA).
Results
Population characteristics
A total of 142 patients fulfilled the inclusion criteria and were approached for the study, of which 79 consented and returned the questionnaire. Only these 79 patients were included in the analysis; the other 63 were excluded. The final study group had a mean age of 50±15 years, of which 58% were female (Table 1). The majority of tumours were confined to the superficial lobe of the parotid gland (89%, n=70) while the remaining patients had a deep lobe parotidectomy (11%, n=9). The dermofat graft was harvested from the iliac region in most patients (97%, n=77) and the remaining patients had a dermofat graft harvested from the periumbilical area (3%, n=2). The most common histopathological tumour types were pleomorphic adenomas (76%, n=60) and Warthin’s tumours (13%, n=10). The mean tumour size was 23±11 mm.
Table 1
| Characteristics | Value (n=79) |
|---|---|
| Age at surgery (years), mean ± SD | 50±15 |
| Gender (male:female), % | 42:58 |
| Years since surgery, median (range) | 3.32 (8.18) |
| Surgery type, n [%] | |
| Superficial | 70 [89] |
| Deep lobe | 9 [11] |
| Dermofat graft donor site, n [%] | |
| Left iliac fossa | 77 [97] |
| Periumbilical | 2 [3] |
| Tumour type, n [%] | |
| Pleomorphic adenoma | 60 [76] |
| Warthin’s tumour | 10 [13] |
| Other† | 9 [11] |
| Tumour size (mm), mean ± SD | 23±11 |
†, basal cell adenoma, oncocytoma, chronic sialadenitis. SD, standard deviation.
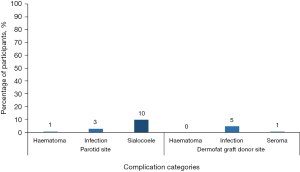
Post-operative complications
The most common recorded complications were parotid sialocoeles (10%, n=8) and dermofat graft donor site infection (5%, n=4) (Figure 2). Two patients (3%) developed a parotid wound infection, one patient (1%) had a parotid haematoma, and a donor site seroma was recorded in one patient (1%). There were no instances of donor site haematoma requiring return to theatre or surgical/radiological intervention.
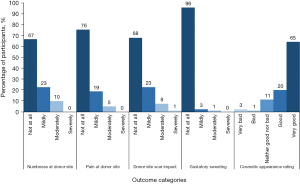
Patient-reported outcomes
Several patients reported experiencing numbness (33%, n=26) or pain (24%, n=19) at the dermofat graft donor site (Figure 3). Those who reported numbness experienced it mildly (23%, n=18) or moderately (10%, n=8). Those with pain experienced it mildly (19%, n=15) or moderately (5%, n=4). Three patients reported experiencing mild (3%, n=2) or moderate (1%, n=1) gustatory sweating. Most patients were satisfied with their post-operative cosmetic appearance (85%, n=67) while a few were not (4%, n=3). The scar at the dermofat graft donor site did not bother most patients (68%, n=54).
Discussion
Dermofat grafting was first described as a reconstructive method in 1931 for a frontal sinus fracture (17). Since then, it has been described in a variety of head and neck surgeries including parotidectomy (14,18,19). Existing reports on the complications and patient satisfaction with this reconstruction method, however, arise from small sample sizes and mixed cohorts (e.g., benign and malignant tumours, total and limited parotidectomies, combined reconstructive methods). This study is the largest Australian-based study dedicated purely to investigating the incidence of post-operative complications and patient-reported outcomes associated with dermofat graft reconstruction in limited parotidectomies for benign parotid disease.
This study demonstrated a low incidence of post-operative complications in patients with dermofat graft reconstruction. Our rates are lower than previously reported findings for donor site haematomas (0–4%), donor site seromas (0–5%), and parotid site haematomas (0–10%) (12,15,19-21). Our study also demonstrated a very low rate of parotid site infections, similar to published literature (19-21). This could be related to the relatively young mean age of our patient population (50 years), possibly reflecting a tendency to perform this procedure on younger patients who are thought to have lower risk of infection or graft-take failure. Our rate of parotid site sialocoeles of 10% is higher than other reported case series in the literature (12,20,21). The reason for this is unclear but may be due to some surgeon protocols of drain removal on Day 1 post-operatively or to an inflammatory effect of the dermofat graft. The risk of sialocoele is also related to tumour size and in our series, the mean tumour size was 23±11 mm (15,22).
One theoretical advantage of using a dermofat graft is potentially a lower risk of developing gustatory sweating or Frey’s syndrome as the graft provides a barrier between the remaining parotid tissue and the overlying skin surface and thus preventing aberrant neural connections between the remaining parotid gland and skin. Three patients in the current study reported experiencing gustatory sweating. This low incidence is consistent with published literature investigating dermofat grafts and Frey’s syndrome (0–4.9%) (12,19-21). Another study that reported a subjective gustatory sweating rate of 19% included malignant tumours and total parotidectomies which are associated with higher rates of developing Frey’s syndrome (23). A multivariate analysis of age, total parotidectomies, and dermofat grafting showed no relationship between dermofat grafting and gustatory sweating (21) whereas another study only found tumour size >4 cm, no disease pathology, resection type, previous radiotherapy or previous parotidectomy, corresponded with the development of Frey’s syndrome (24). While a retrospective cohort study did not find dermofat grafts to reduce Frey’s syndrome significantly compared to no reconstruction or reconstruction with a sternocleidomastoid flap (12), further research is needed into determining whether dermofat grafts are better than other reconstruction methods in preventing Frey’s syndrome.
The main reason for performing dermofat grafting is to resolve the cosmetic defect of hollowing of the side of the face when reconstruction is not performed. Thus, the patient is restored with a normal symmetrical facial cosmesis. Our findings match the high cosmetic satisfaction rates reported in existing literature (12,19,20). Donor site complications perceived by the patients are also similarly low in terms of numbness and bother factor (23), but no other study has reported donor site pain.
The benefits of the dermofat graft reconstruction in parotidectomies include the ease of harvesting technique and short operating time in obtaining the graft compared to other techniques such as a temporoparietal flap (which puts the frontal branch of the facial nerve at risk) and a sternocleidomastoid rotation flap (which puts the spinal accessory nerve at risk). In benign parotid surgery, vascularised free flaps can be avoided unless indicated for extensive resections. Although not the aim of this study, in our experience, placing a dermofat graft does not impair revision parotid surgery and anecdotally makes revision surgery easier as the base of the dermofat graft is able to be lifted off the underlying facial nerve relatively easily with minimal scarring. In our institution, we don’t recommend or utilise dermofat grafts in malignant parotid surgery due to the risk of fat necrosis if adjuvant radiotherapy is used.
Limitations
The external validity of this study is restricted by the inherent limitations of a voluntary survey such as volunteer bias, recall bias, and response bias. We attempted to mitigate this by maximising our sample size through different modes of survey distribution but still obtained relatively low response-to-no-response ratios. However, our cohort is certainly the largest amongst existing reports, which can allow for greater representative analysis. Additionally, further research may expand on this study by incorporating a comparison group so that statistical analyses of significant differences in post-operative outcomes may be ascertained.
Conclusions
Dermofat grafts are a useful reconstructive option for limited parotidectomy defects as they are associated with a low risk of post-operative complications and have a positive patient-reported outcome.
Acknowledgments
The authors would like to acknowledge the assistance of Mr. Kan Gao from Database Manager, Chris O’Brien Lifehouse, who provided administrative support with database management.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://www.theajo.com/article/view/10.21037/10.21037/ajo-23-30/rc
Data Sharing Statement: Available at https://www.theajo.com/article/view/10.21037/ajo-23-30/dss
Peer Review File: Available at https://www.theajo.com/article/view/10.21037/ajo-23-30/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://www.theajo.com/article/view/10.21037/ajo-23-30/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the St Vincent’s Hospital Human Research Ethics Committee (2021/ETH11634) and informed consent was obtained from all participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zhan KY, Khaja SF, Flack AB, et al. Benign Parotid Tumors. Otolaryngol Clin North Am 2016;49:327-42. [Crossref] [PubMed]
- Sanabria A, Kowalski LP, Bradley PJ, et al. Sternocleidomastoid muscle flap in preventing Frey's syndrome after parotidectomy: a systematic review. Head Neck 2012;34:589-98. [Crossref] [PubMed]
- Bianchi B, Ferri A, Ferrari S, et al. Improving esthetic results in benign parotid surgery: statistical evaluation of facelift approach, sternocleidomastoid flap, and superficial musculoaponeurotic system flap application. J Oral Maxillofac Surg 2011;69:1235-41. [Crossref] [PubMed]
- Asal K, Köybaşioğlu A, Inal E, et al. Sternocleidomastoid muscle flap reconstruction during parotidectomy to prevent Frey's syndrome and facial contour deformity. Ear Nose Throat J 2005;84:173-6. [Crossref] [PubMed]
- Taylor SM, Yoo J. Prospective cohort study comparing subcutaneous and sub-superficial musculoaponeurotic system flaps in superficial parotidectomy. J Otolaryngol 2003;32:71-6. [Crossref] [PubMed]
- Cannady SB, Seth R, Fritz MA, et al. Total parotidectomy defect reconstruction using the buried free flap. Otolaryngol Head Neck Surg 2010;143:637-43. [Crossref] [PubMed]
- Demirkan F, Unal S, Arslan E, et al. Versatile anterolateral thigh perforator flap: case of tailored reconstruction for a large temporal and parotidectomy defect. J Reconstr Microsurg 2003;19:221-4. [Crossref] [PubMed]
- Elliott RM, Weinstein GS, Low DW, et al. Reconstruction of complex total parotidectomy defects using the free anterolateral thigh flap: a classification system and algorithm. Ann Plast Surg 2011;66:429-37. [Crossref] [PubMed]
- Epps MT, Cannon CL, Wright MJ, et al. Aesthetic restoration of parotidectomy contour deformity using the supraclavicular artery island flap. Plast Reconstr Surg 2011;127:1925-31. [Crossref] [PubMed]
- Teknos TN, Nussenbaum B, Bradford CR, et al. Reconstruction of complex parotidectomy defects using the lateral arm free tissue transfer. Otolaryngol Head Neck Surg 2003;129:183-91. [Crossref] [PubMed]
- Valentini V, Cassoni A, Marianetti TM, et al. Anterolateral thigh flap for the reconstruction of head and neck defects: alternative or replacement of the radial forearm flap? J Craniofac Surg 2008;19:1148-53. [Crossref] [PubMed]
- Fasolis M, Zavattero E, Iaquinta C, et al. Dermofat graft after superficial parotidectomy to prevent Frey syndrome and depressed deformity. J Craniofac Surg 2013;24:1260-2. [Crossref] [PubMed]
- Mashrah MA, Aldhohrah T, Abdelrehem A, et al. What is the best method for prevention of postparotidectomy Frey syndrome? Network meta-analysis. Head Neck 2021;43:1345-58. [Crossref] [PubMed]
- Harada T, Inoue T, Harashina T, et al. Dermis-fat graft after parotidectomy to prevent Frey's syndrome and the concave deformity. Ann Plast Surg 1993;31:450-2. [Crossref] [PubMed]
- Petrides GA, Subramaniam N, Pham M, et al. Reducing the morbidity of parotidectomy for benign pathology. ANZ J Surg 2020;90:2315-21. [Crossref] [PubMed]
- Chandarana S, Fung K, Franklin JH, et al. Effect of autologous platelet adhesives on dermal fat graft resorption following reconstruction of a superficial parotidectomy defect: a double-blinded prospective trial. Head Neck 2009;31:521-30. [Crossref] [PubMed]
- Figi FA. Depression of frontal region, fat transplant. Surg Clin North Am 1931;11:8-31.
- Nosan DK, Ochi JW, Davidson TM. Preservation of facial contour during parotidectomy. Otolaryngol Head Neck Surg 1991;104:293-8. [Crossref] [PubMed]
- Pham M, Eviston TJ, Clark JR. Reconstruction of limited parotidectomy defects using the dermofat graft. ANZ J Surg 2017;87:E256-60. [Crossref] [PubMed]
- Baum SH, Pförtner R, Ladwein F, et al. Use of dermis-fat grafts in the prevention of Frey's syndrome after parotidectomy. J Craniomaxillofac Surg 2016;44:301-8. [Crossref] [PubMed]
- Gruszczynski NR, Anderies BJ, Dey JK, et al. Analysis of Abdominal Dermal-Fat Grafting to Repair Parotidectomy Defects: An 18-Year Cohort Study. Laryngoscope 2020;130:2144-7. [Crossref] [PubMed]
- Kim BS, Kim MR, Kim YW, et al. Risk factors for sialocele after parotidectomy: Does tumor size really matter? Auris Nasus Larynx 2023;50:935-41. [Crossref] [PubMed]
- Mianroodi AA, Mohtashami S, Romero N, et al. Autologous Free Dermal-Fat-Fascial Graft for Parotidectomy Defects: A Case Series. Ann Otol Rhinol Laryngol 2021;130:1171-80. [Crossref] [PubMed]
- Lee CC, Chan RC, Chan JY. Predictors for Frey Syndrome Development After Parotidectomy. Ann Plast Surg 2017;79:39-41. [Crossref] [PubMed]
Cite this article as: Khoo AL, Clark JR, Low TH(, Wykes J, Ch’ng S, Elliott M. Functional and aesthetic outcomes of dermofat graft reconstruction in limited parotidectomy defects: a cross-sectional study. Aust J Otolaryngol 2024;7:13.