Enhancing epistaxis blood loss estimation with an online visual aid
Introduction
Epistaxis is a common presentation to Emergency Departments and General Practitioners with an estimated lifetime prevalence of 60% in the United States population (1). With the advent of novel anti-coagulation therapy and in patients with multiple comorbidities, blood loss can have quite significant consequences. For other patients, correct estimation of blood loss can guide more judicious resuscitation, avoid unnecessary blood transfusions, and preserve transfusion supplies. Estimations of blood loss in obstetric and colorectal surgery are well described and similar studies in post-partum haemorrhage have suggested that exposure to visual aids of blood loss can improve clinician estimations (2-5). However, no validated or investigated guide exists for describing blood volume loss in epistaxis or other otolaryngology-related bleeding. (1). A previous systematic review and meta-analysis, conducted by the lead investigator and published in 2020, found that blood loss in epistaxis was reliably overestimated; however, with increasing years of experience, estimation improved (6). The purpose of this follow-up study was to see if experience could be taught by aiming to quantify the ability of healthcare professionals to estimate blood loss in epistaxis pre- and post-visual aid education. We hypothesised that post-education and exposure, reliability would improve.
Methods
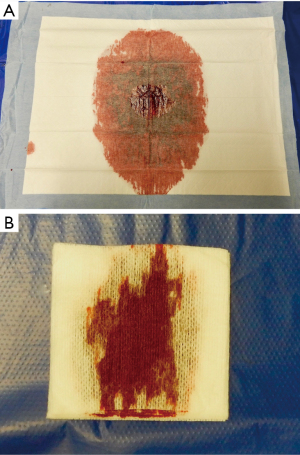
Participants were clinical staff affiliated with a metropolitan Australian hospital. The production of the visual aid was formulated from the initial project published in 2020. It was derived from photographs taken of porcine blood spilt on common household and medical products. Those items included a white T-shirt, a pile of ten tissues, a white towel, a pair of men’s underwear, a white sheet on a single mattress, a single pack of rayteks (a non-woven gauze used commonly in surgery) and a bluey (an absorbent pad with a waterproof backing used in a hospital setting) (see Figure 1). The T-shirt and ten tissues were selected as the base items for review as, in the authors experience, patients commonly present with blood loss on these items. A double-page visual aid pictogram was developed from the initial study and made available (see Appendix 1). The pictogram included a total of five pictures on each page of increasing volume/s of blood loss on both a white T-shirt and ten household tissues. The visual aid appeared as an intermission between the two surveys (SurveyMonkey®) and then participants were asked to complete the survey post a single viewing of the visual aid. The survey was distributed via the medical workforce to all clinicians employed at a single hospital. The survey was delivered online in accordance with coronavirus disease 2019 (COVID-19) restrictions at the time.
Basic demographic details, including area of specialty, and length of employment, were gathered. The actual volumes spilt on the ten products are seen in Table 1; these were taken from the primary study and several items were duplicated with two different volumes to highlight the visual change with increasing volumes of blood; for example, bluey 1 and 2, T-shirt 1 and 2 and mattress 1 and 2. A sliding number scale was used by participants to select the exact estimated volume to the nearest millilitre. All photographs had a centimetre scale for reference of object size.
Table 1
| Object | Actual volume (mL) | Pre mean (95% CI) |
Pre actual mean difference (95% CI) |
P | Post mean (95% CI) |
Post actual mean difference (95% CI) |
P | Pre-post mean difference (95% CI) |
P |
|---|---|---|---|---|---|---|---|---|---|
| Rayteks | 30 | 40.46 (35.88, 45.04) | 10.46 (5.87, 15.05) | <0.001 | 32.11 (26.90, 37.32) | 1.66 (−3.41, 6.74) | 0.521 | −8.35 (−13.63, −3.07) | 0.002 |
| Tissues | 20 | 13.79 (11.90, 15.69) | −6.21 (−8.23, −4.18) | <0.001 | 15.66 (13.43, 17.88) | −4.40 (−6.64, −2.17) | <0.001 | 1.87 (−0.76, 4.49) | 0.163 |
| Bluey 1 | 50 | 222.64 (196.10, 249.19) | 172.64 (144.59, 200.69) | <0.001 | 53.11 (25.70, 80.51) | 2.28 (−26.35, 30.90) | 0.876 | −169.54 (−200.80, −138.27) | <0.001 |
| Bluey 2 | 10 | 221.50 (195.39, 247.61) | 211.50 (186.42, 236.58) | <0.001 | 41.75 (15.64, 67.86) | 31.75 (6.67, 56.83) | 0.013 | −179.75 (−213.66, −145.84) | <0.001 |
| U/wear | 50 | 40.93 (34.72, 47.14) | −9.07 (−15.20, −2.94) | 0.004 | 38.23 (31.11, 45.35) | −12.82 (−19.69, −5.95) | <0.001 | −2.70 (−9.71, 4.32) | 0.451 |
| Sheet 1 | 50 | 149.06 (38.16, 259.96) | 99.06 (−23.18, 221.30) | 0.112 | 1,636.98 (1,522.72, 1,751.23) | 1,586.92 (1,462.65, 1,711.19) | <0.001 | 1,487.92 (1,338.60, 1,637.23) | <0.001 |
| Sheet 2 | 1,000 | 130.00 (14.14, 245.86) | −870.00 (−981.11, −758.89) | <0.001 | 1,583.63 (1,466.82, 1,700.44) | 583.29 (471.60, 694.98) | <0.001 | 1,453.63 (1,302.34, 1,604.92) | <0.001 |
| T-shirt 1 | 100 | 171.83 (110.13, 233.53) | 71.83 (9.78, 133.88) | 0.023 | 697.36 (635.03, 759.69) | 597.37 (534.85, 659.88) | <0.001 | 525.53 (458.30, 592.75) | <0.001 |
| T-shirt 2 | 500 | 166.83 (107.64, 226.03) | −333.17 (−388.97, −277.36) | <0.001 | 697.48 (637.81, 757.14) | 197.06 (140.95, 253.16) | <0.001 | 530.65 (457.20, 604.09) | <0.001 |
| Towel | 250 | 260.50 (229.03, 291.97) | 10.50 (−21.48, 42.48) | 0.520 | 256.63 (220.46, 292.80) | 5.86 (−29.25, 40.96) | 0.744 | −3.87 (−44.91, 37.17) | 0.853 |
CI, confidence interval.
The accuracy of a participant to estimate the blood loss on an individual item was assessed pre- and post-education. Sample descriptives consisted of frequency distributions by category. Pre-post estimated means, pre-post changes and differences from actual volume were calculated for each object using linear mixed models. Results were summarised using marginal means and 95% confidence intervals (CIs). Stata version 17 [StataCorp (RRID: SCR_012763), College Station, TX, USA] was used for data analysis and significance levels (alpha) were set at 0.05.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethics approval was obtained from the local site Human Research Ethics Committee (HREC2020/ETH/2011), and informed consent was taken from all individual participants.
Results
The survey was sent by the hospital administration to all emergency department (medical and nursing staff) and junior medical workforce staff (interns/residents and registrars). There were 87 respondents to the survey. More than 90% were doctors with the remainder consisting of nursing staff. A third worked in the emergency department and a third were in their first post graduate years (intern or resident). One participant worked in anaesthetics and one in general practice. Almost 20% had worked for more than 10 years as a clinician as seen in Table 2. The median time to complete the survey was 5 minutes and 59 seconds.
Table 2
| Factors | Category | N (%) |
|---|---|---|
| Profession | Doctor | 79 (90.8) |
| Nurse | 8 (9.2) | |
| Specialisation | Emergency Medicine | 27 (31.0) |
| Medical | 9 (10.3) | |
| Other | 2 (2.3) | |
| Rotation (i.e., intern/resident) | 30 (34.5) | |
| Surgical | 11 (12.6) | |
| Years of experience | 0–<3 years | 43 (49.4) |
| 3–<5 years | 18 (20.7) | |
| 5–<10 years | 9 (10.3) | |
| ≥10 years | 17 (19.5) |
Overall estimation of each object was reviewed and compared to pre- and post-visual aid utilisation (see Table 1). Items that were more reliably estimated post-visual aid demonstrated no statistical significance between the actual volume and post-education volume (P>0.05).
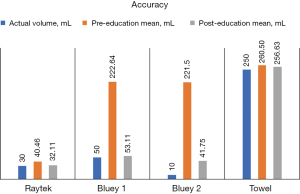
In this study, the amount of blood spilt on the rayteks, a universal medical and surgical product had improved estimation of the blood volume spilt post the visual aid education (actual volume: 30 mL, pre-education: 40.46 mL, post-education: 32.11 mL, P=0.521) (see Figure 2). Likewise, with the 50 mL bluey the estimated mean blood volume was improved post-education when compared to the actual volume (actual volume: 50 mL, pre-education: 222.64 mL, post-education: 53.11 mL, P<0.876). This was seen across all years of experience (see Table 3). The 10-mL bluey had improved accuracy pre- and post-education (221.5 vs. 41.75, P=0.013) but when compared to the actual volume post-education was still over-estimated (P>0.001).
Table 3
| Factors | Category | Pre mean (95% CI) | Post mean (95% CI) | Mean difference (95% CI) | P |
|---|---|---|---|---|---|
| All | – | 222.64 (196.10, 249.19) | 53.11 (25.70, 80.51) | −169.54 (−200.80, −138.27) | <0.001 |
| Profession | Doctor | 218.73 (190.95, 246.51) | 51.84 (23.06, 80.61) | −166.90 (−199.74, −134.06) | <0.001 |
| Nurse | 261.25 (173.95, 348.55) | 65.63 (−21.67, 152.92) | −195.63 (−296.11, −95.14) | <0.001 | |
| Specialisation | Emergency Medicine | 174.44 (129.23, 219.66) | 37.89 (−8.10, 83.88) | −136.56 (−190.19, −82.93) | <0.001 |
| Medical | 321.11 (242.80, 399.42) | 71.67 (−6.64, 149.98) | −249.44 (−341.18, −157.71) | <0.001 | |
| Other (n=2) | 135.00 (−31.12, 301.12) | 37.50 (−128.62, 203.62) | −97.50 (−292.11, 97.11) | 0.326 | |
| Rotation | 257.33 (214.44, 300.22) | 63.57 (16.97, 110.17) | −193.77 (−247.21, −140.32) | <0.001 | |
| Surgical | 153.64 (82.80, 224.47) | 39.55 (−31.29, 110.38) | −114.09 (−197.07, −31.11) | 0.007 | |
| Years of experience | 0–<3 years | 260.70 (224.15, 297.25) | 63.01 (24.83, 101.19) | −197.69 (−241.31, −154.06) | <0.001 |
| 3–<5 years | 220.00 (163.51, 276.49) | 45.21 (−14.34, 104.76) | −174.79 (−242.69, −106.89) | <0.001 | |
| 5–<10 years | 160.00 (80.11, 239.89) | 35.56 (−44.33, 115.45) | −124.44 (−216.70, −32.19) | 0.008 | |
| ≥10 years | 162.35 (104.22, 220.48) | 44.12 (−14.01, 102.25) | −118.24 (−185.36, −51.11) | 0.001 |
CI, confidence interval.
The underwear was underestimated both pre- and post-education (actual: 50 mL, pre-mean: 40.93 mL, post-mean: 38.23 mL).
Results for household items that were shown twice include both the sheet, towel, and T-shirt. The sheet with 1,000 mL of blood spilt on it; this was estimated with a mean volume of 130 mL pre-education and post-education was 1,583.63 mL (pre-post mean difference 1,453.63, P<0.001). The sheet with 50 mL was more accurate pre-education with a pre-exposure mean of 149.06 with a significant over-estimation with a post-exposure mean of 1,636.98 (95% CI: 1,522.72–1,751.23, P<0.001).
The T-shirt with 500 mL of blood spilt on it was underestimated pre-education regardless of profession or years of experience with a pre-exposure mean estimation of 166.83 (95% CI: 107.64–226.03). Post-exposure to the visual aid this item was overestimated with a post-exposure mean of 697.48 (95% CI: 637.81–757.14) (see Table 4). The T-shirt with 100 mL of blood spilt on it had a larger difference post-education then pre (post mean 697.36 vs. pre mean 171.83) with both still significantly different to the actual volume (pre-post mean difference 525.53, P<0.001).
Table 4
| Factors | Category | Pre mean (95% CI) | Post mean (95% CI) | Mean difference (95% CI) | P |
|---|---|---|---|---|---|
| All | – | 166.83 (107.64, 226.03) | 697.48 (637.81, 757.14) | 530.65 (457.20, 604.09) | <0.001 |
| Profession | Doctor | 164.63 (104.28, 224.98) | 669.29 (608.41, 730.18) | 504.66 (429.94, 579.39) | <0.001 |
| Nurse | 186.67 (5.61, 367.73) | 946.67 (765.61, 1,127.73) | 760.00 (537.14, 982.86) | <0.001 | |
| Specialisation | Emergency Medicine | 160.53 (64.00, 257.05) | 681.05 (584.52, 777.58) | 520.53 (397.58, 643.47) | <0.001 |
| Medical | 141.67 (−30.11, 313.44) | 588.33 (416.56, 760.11) | 446.67 (227.88, 665.45) | <0.001 | |
| Other (n=2) | 175.00 (−122.52, 472.52) | 475.00 (177.48, 772.52) | 300.00 (−78.94, 678.94) | 0.121 | |
| Rotation | 192.78 (93.60, 291.95) | 760.46 (658.51, 862.41) | 567.68 (439.18, 696.19) | <0.001 | |
| Surgical | 130.00 (−10.25, 270.25) | 567.78 (427.53, 708.03) | 437.78 (259.14, 616.41) | <0.001 | |
| Years of experience | 0–<3 years | 196.92 (111.55, 282.30) | 740.77 (655.39, 826.15) | 543.85 (437.63, 650.07) | <0.001 |
| 3–<5 years | 142.50 (16.83, 268.17) | 672.24 (541.26, 803.22) | 529.74 (369.09, 690.39) | <0.001 | |
| 5–<10 years | 122.86 (−41.69, 287.40) | 437.14 (272.60, 601.69) | 314.29 (109.57, 519.00) | 0.003 | |
| ≥10 years | 154.67 (42.26, 267.07) | 762.67 (650.26, 875.07) | 608.00 (468.16, 747.84) | <0.001 |
CI, confidence interval.
The towel household item with 250 mL of blood spilt was estimated accurately both pre- and post-education [pre mean 260.50 (95% CI: 229.03–291.97)/post mean 256.63 (95% CI: 220.46–292.80), P=0.744] (see Figure 1).
Discussion
This study examined the reliability of estimation of blood loss amongst clinicians in epistaxis post-visual aid education. Blood loss is a universal presenting complaint to emergency departments as well as experienced in operating rooms throughout the world. Visual estimation is a useful adjunct to patient assessment as it does not rely on equipment that may not be universally available and can be used at the point of care.
A reliable estimation of blood loss can lead to appropriate resuscitation and distribution of health resources (7). Furthermore, estimation of blood loss intraoperatively can guide management, including intraoperative fluid replacement and surgical duration. In otolaryngology, endoscopic sinus surgery is a common procedure but even in non-oncologic cases can result in significant blood loss. A recent American study demonstrated that intraoperative assessment of blood loss in functional endoscopic sinus surgery (i.e., iatrogenic epistaxis) was under-estimated in 75% of cases (8).
From the pilot study, results indicated that blood loss is poorly estimated; particularly in larger volumes; and there was a significant increase in accuracy in blood loss estimation with increasing years of clinical experience (6). A visual aid tool could improve the estimation of blood loss and be used as a measurement and reference tool by primary care physicians and first responders. By comparing pre- and post-education estimations, this tool could be validated for widespread use.
A recently published paper found that visual estimation of blood loss on medical sponges is poorly undertaken, however this was not the case in our study (9). Both the rayteks and bluey estimations were more accurate post-education across all durations of clinical experience. This has applicability in education for both surgical and non-surgical staff as both items are found in basic cannulation packs in the emergency department and wards as well as surgical setups respectively. This is comparable with previous studies in the obstetric field which supports that no prior experience is required to supplement the visual aid (2,3,10,11). As in the investigators first study, this second cohort also underestimated the amount of blood spilt on underwear; this item is described in per rectal bleeding however seen less frequently in otolaryngology clinical experience (6).
The use of household products was designed to capture estimation of blood loss in the community should patients/caregivers bring in items with blood loss on for pictorial assessment. In this study, such items including sheet and T-shirt were underestimated pre-education and overestimated post-education. Due to the variety of items that patients may present with and with likely varying absorbent capacities, the use of a sheet and T-shirt as the visual aid may be difficult to interpret.
In the United States where blood loss due to traumatic injury is a major cause of death, a campaign called Stop the Bleed® was designed to teach the general public to recognise and stop life threatening blood loss in the community (12). This was designed to guide importance of timely medical attention and/or resuscitation and based on evidence that brief and easily accessible web-based educational programs have better retention rates than in person teaching (13). This supports the improvement in estimation of blood loss in epistaxis post our online educational packet. The average time to complete this survey was just over 5 minutes compared to the pilot study which took 3 minutes. This demonstrates that only a brief example of volumetric blood loss increases estimation.
There are several limitations of this study. Previous studies on blood loss education in the postpartum setting have been conducted in small group settings. Due to the timing of the survey rollout during the COVID-19 pandemic, face-to-face education of the visual aid was restricted. This also limited the ability of the participants to view the visual aid throughout the survey for reference repeatedly as the surveys were in sequence and the visual aid could not be viewed whilst the post-education survey was completed. In clinical practice it is more likely that clinical staff could view the visual aid simultaneously. The survey was emailed to all junior medical staff and emergency department staff at a single metropolitan hospital. Given an opt-in participation this blanket delivery could have resulted in selection bias for those who had a vested interest in blood loss estimation thereby potentially excluding those with less experience or exposure.
Only two items were selected for the education, the white T-shirt and tissues, as these were thought to be universally applicable for patients presenting with Ear, Nose and Throat haemorrhage. The T-shirt had similar post-exposure estimations for both the 100- and 500-mL objects; since the T-shirt item was lying down this might have changed the perception of absorption (i.e., two layers of the item soaked through). Furthermore, the visual aid included these same photos as well as other increasing volumes of blood. This could have confounded the participants as the same images were viewed during the survey as well as the visual aid.
The ideal long term practical application of this visual aid is an electronic format that can be viewed at the point of care of a patient with blood loss such as a telephone app or electronic flyer. Medical items such as rayteks and blueys could be included as universal healthcare products that demonstrated improved accuracy in estimation post brief visual aid exposure as shown in this study.
Conclusions
Blood loss in otolaryngology has presentations both emergently and in the operating room. The ability to accurately estimate blood loss has physiological and resource allocation implications. Based on the primary study designed by this author, experience improved accuracy and this follow-up study demonstrated improvement in blood loss estimation with brief online education in blood loss seen on common medical products.
Acknowledgments
Funding: None.
Footnote
Data Sharing Statement: Available at https://www.theajo.com/article/view/10.21037/ajo-23-36/dss
Peer Review File: Available at https://www.theajo.com/article/view/10.21037/ajo-23-36/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://www.theajo.com/article/view/10.21037/ajo-23-36/coif). P.F. serves as an unpaid editorial board member of Australian Journal of Otolaryngology. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethics approval was obtained from the local site Human Research Ethics Committee (HREC2020/ETH/2011), and informed consent was taken from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Epistaxis Seikaly H. N Engl J Med 2021;384:944-51. [Crossref] [PubMed]
- Schorn MN. Measurement of blood loss: review of the literature. J Midwifery Womens Health 2010;55:20-7. [Crossref] [PubMed]
- Parayre I, Rivière O, Debost-Legrand A, et al. Reliability of student midwives' visual estimate of blood loss in the immediate postpartum period: a cross-sectional study. Int J Nurs Stud 2015;52:1798-803. [Crossref] [PubMed]
- Natrella M, Di Naro E, Loverro M, et al. The more you lose the more you miss: accuracy of postpartum blood loss visual estimation. A systematic review of the literature. J Matern Fetal Neonatal Med 2018;31:106-15. [Crossref] [PubMed]
- Budair B, Ahmed U, Hodson J, et al. Are we all guilty of under-estimating intra-operative blood loss during hip fracture surgery? J Orthop 2016;14:81-4. [Crossref] [PubMed]
- Grigg S, Maunder J, Betz-Stablein B, et al. Reliability of estimating blood loss in epistaxis. Aust J Otolaryngol 2020;3:15. [Crossref]
- Gerdessen L, Meybohm P, Choorapoikayil S, et al. Comparison of common perioperative blood loss estimation techniques: a systematic review and meta-analysis. J Clin Monit Comput 2021;35:245-58. [Crossref] [PubMed]
- Eliason MJ. Estimated versus actual; The accuracy of accounting for blood loss during endoscopic sinus surgery. Am J Otolaryngol 2020;41:102342. [Crossref] [PubMed]
- Piekarski F, Gerdessen L, Schmitt E, et al. Do we visually estimate intra-operative blood loss better with white or green sponges and is the deviation from the real blood loss clinically acceptable? Results from a simulated scenario study. PLoS One 2020;15:e0240808. [Crossref] [PubMed]
- Glover P. Blood loss at delivery: how accurate is your estimation? Aust J Midwifery 2003;16:21-4. [Crossref] [PubMed]
- Tebruegge M, Misra I, Pantazidou A, et al. Estimating blood loss: comparative study of the accuracy of parents and health care professionals. Pediatrics 2009;124:e729-36. [Crossref] [PubMed]
- Prytz E, Phillips R, Lönnqvist S, et al. Laypeople perception and interpretation of simulated life-threatening bleeding: a controlled experimental study. BMC Emerg Med 2021;21:100. [Crossref] [PubMed]
- Goolsby CA, Strauss-Riggs K, Klimczak V, et al. Brief, Web-based Education Improves Lay Rescuer Application of a Tourniquet to Control Life-threatening Bleeding. AEM Educ Train 2018;2:154-61. [Crossref] [PubMed]
Cite this article as: Grigg S, Moriarty A, Jacques A, Friedland P. Enhancing epistaxis blood loss estimation with an online visual aid. Aust J Otolaryngol 2024;7:3.