Contemporary management of tonsillar schwannoma—a systematic review
Introduction
Neurogenic tumours make up a small percentage of neoplastic head and neck lesions and mainly comprise neurofibromas and schwannomas (also known as neurilemmomas) (1). Schwannomas are benign, encapsulated tumours of Schwann cells in peripheral nerves (2). Histopathological assessment of schwannomas identifies two classic cellular patterns: (I) Antoni A areas characterised by increased cellularity and spindle nuclei; and (II) Antoni B areas characterised by a loose arrangement of cells that are hypocellular and have variable macrophage infiltrate (3,4). Other features include Verocay bodies, hyalinised vessels with perivascular haemosiderin deposition, cystic spaces and degenerative changes (3).
The risk factors for the development of these lesions are prior radiation exposure and genetic predisposition (2), such as Von Recklinghausen’s disease and type I neurofibromatosis (5).
The head and neck region is the most common site for schwannomas (25–48% of cases), but only about one percent occur intraorally (6). They mostly involve the acoustic nerve (7) and but can also occur in the trigeminal, facial and hypoglossal nerves (8). The first case of tonsillar schwannoma was described in the literature in 1975 (9) and since then there have only been twelve other cases reported worldwide in the English literature. Differential diagnoses for unilateral tonsillar hypertrophy include infectious (tonsillitis, peritonsillar abscess), inflammatory (Kawasaki disease, Kimura’s disease) and neoplastic lesions, both benign (polyp, squamous papilloma, haemangioma) and malignant (squamous cell carcinoma, lymphoma) (10-12). Current literature on tonsillar schwannoma consists mainly of case reports, with no clear guidelines for workup and management of this rare disease. This systematic review summarises the clinical features, diagnostic workup and management, with the aim of providing guidance for the treatment of palatine tonsil schwannomas. We present this article in accordance with the PRISMA reporting checklist (available at https://www.theajo.com/article/view/10.21037/ajo-23-31/rc).
Methods
Study design
A systematic review of the literature was performed in relation to tonsillar schwannoma.
Search strategies
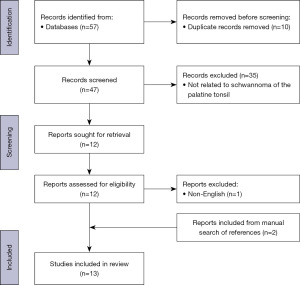
A review of the published literature was performed on 5th May 2023 (Figure 1). Embase, Medline and PubMed databases were searched for eligible studies. Four main search terms were combined with the Boolean operators “AND’ and “OR”. The keywords within the first two searches were “tonsil” OR “palatine tonsil”. The second two searches were “schwannoma” OR “neurilemmoma”. Both searches were combined with the Boolean operator “AND”. All cases fulfilling the search criteria were reviewed by the author and relevant cases were compiled into a database. The study was not registered prior to completion and a review protocol was not prepared.
Study inclusion/exclusion criteria
Cases with a diagnosis of palatine tonsil schwannoma were included in the study. Both adult and paediatric cases were included. Cases that did not have a diagnosis of schwannoma of the palatine tonsil were excluded, for example schwannomas of other regions in the head and neck or oral cavity. Duplicate and non-English cases were excluded.
Study selection
Search strategies were implemented by author S.A.K. and results were collated into a Microsoft Excel spreadsheet. Duplicate references were removed via manual search. Remaining titles were screened for eligibility against inclusion and exclusion criteria. The bibliographies of the relevant studies were reviewed to identify additional relevant studies. The final list of articles included thirteen case reports and was reviewed by C.M., senior author and fellowship trained Otolaryngologist.
Data extraction
Study data included year of publication, age and sex of patient, presenting symptoms, clinical examination findings, imaging modality and results, biopsy results, histopathology results, surgical technique and follow-up interval and outcome.
Quality/risk of bias
Risk of bias was assessed using the Joanna Briggs Institute (JBI) checklist standardised tool developed for case reports, which includes eight questions (13)—the detailed assessment of each study can be found in the supplementary appendix online.
Statistical analysis
Due to the small number of cases, a meta-analysis of the data was not possible. A descriptive statistical analysis and qualitative review of the data collected was conducted using Microsoft Excel.
Results
Patient demographics
The age range of patients presenting with tonsillar schwannoma is between eight to seventy-four years of age, with an average age of thirty-seven years. There were only three paediatric cases and it appears to affect females (nine cases) (6,7,14-20) more than males (four cases) (8,9,21,22) (Table 1).
Table 1
| Ref | Authors | Year | Age, year | Sex | Presenting complaint | Side | CL | Biopsy | Imaging | Surgical approach | Recurrence |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (8) | Anil et al. | 2005 | 38 | M | DWS | Left | N | FNA | USS, CT | Tonsillectomy | Nil at 18 months |
| (14) | Bildirici et al. | 2002 | 69 | F | IFM | Right | N | FNA | MRI | Tonsillectomy | Nil at 12 months |
| (6) | Boujguenna et al. |
2022 | 74 | F | DWS | Left | N | Y | CT | Tonsillectomy | Unknown |
| (15) | Chaudhary | 2011 | 42 | F | IFM | Right | N | FNA | CT | Tonsillotomy | Nil at 12 months |
| (21) | Datta et al. | 2020 | 42 | M | Pain | Left | N | N | CT | Tonsillectomy | Nil at 1 month |
| (16) | Goto et al. | 2012 | 44 | F | IFM | Right | N | Y | CT | Tonsillectomy | Nil at 11 months |
| (22) | Joseph et al. | 2010 | 24 | M | IFM | Right | N | Y | CT | Tonsillotomy | Nil at 2 weeks |
| (17) | Lall et al. | 1999 | 13 | F | DWS | Left | N | N | Nil | Tonsillectomy | Nil recurrence |
| (7) | Lee et al. | 2007 | 23 | F | IFM | Left | N | N | CT | Tonsillectomy | Nil recurrence |
| (9) | Naik et al. | 1975 | 45 | M | Foreign body sensation | Right | N | N | Nil | Tonsillectomy | Unknown |
| (18) | Pham et al. | 2013 | 8 | F | DWS | Right | N | N | Nil | Tonsillotomy | Nil at 5 months |
| (19) | Piplani et al. | 2011 | 14 | F | Pain | Right | N | N | Nil | Bilateral tonsillectomy | Nil recurrence |
| (20) | Ruan et al. | 2008 | 37 | F | IFM | Right | N | N | CT | Tonsillectomy | Unknown |
CL, cervical lymphadenopathy; M, male; F, female; DWS, difficulty with swallowing; IFM, initially found mass; N, no; FNA, fine needle aspiration; Y, yes; USS, ultrasound scan; CT, computed tomography; MRI, magnetic resonance imaging; Nil, no recurrence at specified follow-up.
Presenting symptoms
Most patients with tonsillar schwannoma present with either progressive dysphagia due to mass effect of the lesion (6,8,17,18) or notice an enlarging unilateral mass on intraoral self-examination (7,14-16,20,22). Other presenting symptoms include throat pain (19,21) and sensation of a foreign body (9). Associated symptoms included dysphonia, odynophagia, weight loss, referred pain to the ipsilateral ear, snoring and symptoms of obstructive sleep apnoea (OSA).
Clinical appearance
The general appearance of tonsillar schwannomas on clinical examination is a smooth, spherical, or ovaloid mass that projects into the pharyngeal cavity. It is non-tender and has a firm consistency. It is not fluctuant and there is no ulceration of the mucosa. The tumour is attached to the nerve of origin but remains mobile (17). These findings have been described as unilateral. One case reported bilateral abnormalities with one tonsil larger than the other, however schwannoma was only found in the larger tonsil (19). The lesions have been described as extending into the ipsilateral tongue base, nasopharynx, oropharynx and through the midline. Schwannoma was found in the right tonsil in eight cases (9,14-16,18-20,22) and in the left tonsil in five cases (6-8,17,21).
Cervical lymphadenopathy
There has been no documented cervical lymphadenopathy associated with tonsillar schwannomas.
Biopsy
Three patients had fine needle aspiration biopsies performed pre-operatively and the cytology for each specimen yielded a non-diagnostic result (8,14,15). In the case study by Joseph et al. [2010] (22), an incisional biopsy was performed in an outpatient clinic setting under local anaesthetic and yielded a histopathological result for a benign schwannoma.
Histopathology
Histopathological analysis of tonsillar schwannomas showed classical features—spindle cells arranged in Antoni A and Antoni B areas with Verocay bodies. Other features described include degenerative changes, such as perivascular hyalinisation and large dilated vessels. In this review, there was only one case of malignant tonsillar schwannoma which showed “mitoses of six per ten fields” and local infiltration (6).
Imaging
The majority of cases utilised computed tomography (CT) and described a well circumscribed, heterogenous lesion in the area of the tonsil on plain CT (6-8,15,16,20-22). Contrast-enhanced CT showed a heterogeneously enhanced mass, without enhancement of the capsule (20). There was no infiltration or lymph node enlargement seen on any of the imaging performed.
Other imaging modalities used included transoral ultrasound and magnetic resonance imaging (MRI). On ultrasound the lesion appeared as a “hypovascular mass with or without central necrosis” (8). On MRI, tonsillar schwannomas appear as “well circumscribed, hypointense lesions on T1-weighted images, and hyperintense on T2-weighted images” (14).
Management
Ten out of the thirteen cases reported were treated with tonsillectomy of the abnormal tonsil only (6-9,14,16,17,19-21). Three cases performed a wide local excision of the tumour only and did not remove the entire affected tonsil (15,18,22). One of these cases reported an incomplete resection of the schwannoma, however there was no evidence of lymphoma or malignancy in the excised tissue, therefore a re-excision was not performed (18). In one case the patient underwent a bilateral tonsillectomy as both tonsils looked abnormal upon clinical examination, however only the larger, right tonsil was found to have schwannoma (19). There were no intra-operative or post-operative complications reported in any of the cases published.
Functional deficits
There were no functional deficits reported immediately post-operatively or at follow-up.
Recurrence
Seven cases discussed follow-up at a specific post-operative interval, ranging between two weeks and eighteen months (8,14-16,18,21,22). Three cases did not specify a particular interval for post-operative follow-up (7,17,19) and three cases did not discuss follow-up at all (6,9,20). There was no recurrence of the schwannoma at follow-up. Patients were only followed-up once post-operatively and there was no regular surveillance as part of their management plan.
Discussion
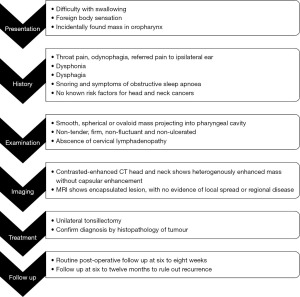
Based on the management of the thirteen cases of tonsillar schwannoma worldwide we propose a management algorithm as outlined below (Figure 2). Presentation of a unilateral tonsillar mass is usually considered malignant until proven otherwise, thus a thorough history and examination will determine the level of clinical suspicion. Malignant transformation of schwannomas is exceedingly rare, however if present, has a poor prognosis, high rate of recurrence and metastases and is fatal (23,24).
Both imaging modalities—CT and MRI—provides useful information and helps to differentiate between invasive, malignant, and benign lesions, however neither are diagnostic for schwannomas. Features of schwannomas on CT in other areas of the body are consistent with the histopathological variations, for example Antoni A are represented as high density areas on CT whilst Antoni B, old haemorrhage and cystic changes are seen as low-density areas (20). This is consistent with the heterogenous appearance of tonsillar schwannomas on CT (25).
The imaging of choice is dependent on the resources available at the institution.
The accuracy of fine needle aspiration cytology in diagnosing other head and neck schwannomas is low, between 18% and 33% and is dependent on the specimen quality and the experience of the Cytopathologist (2). Incisional biopsies have an accuracy rate of 45.8%, however have the risks of: (I) insufficient sample; (II) exposing the patient to at least two procedures (i.e., first incision biopsy and then excision of the tumour); and (III) causing scar tissue to form at the surgical site, potentially making subsequent procedures more difficult (2). Biopsy of lesions yield unreliable results and exposes patients to two procedures and an increased level of associated risk. Therefore, pre-operative biopsy is not required in the workup of tonsillar schwannomas.
Ultimately, unilateral tonsillectomy is both a diagnostic and therapeutic procedure in this condition. All cases employed traditional tonsillectomy techniques to remove the schwannoma. However, transoral robotic surgery (TORS) is becoming a favourable method for removing tonsillar neoplasms due to better access of the pharynx for resection compared to traditional tonsillectomy and better post-operative outcomes compared to open approaches (26). In particular, radical tonsillectomy using TORS is an effective method for removing tonsillar carcinomas that have extended into surrounding areas or if there is limited transoral access and has reduced morbidity compared to open surgical approaches (27).
The surgical management of extracranial head and neck schwannomas in other locations is based on weighing the risks and benefits of surgery, pre-operative symptoms, and the anticipated severity of post-operative neurological deficits. Complete resection of the tumour results in palsy of the associated nerve, however with intracapsular enucleation only 31% of patient have a post-operative nerve palsy at six-month follow up—there is no difference in the recurrence rates (0% at two years) between the two methods (28). The risk of nerve palsy post-tonsillectomy is exceedingly rare, but may affect the glossopharyngeal nerve resulting in referred otalgia and transient dysgeusia (29). Tonsillectomy is the treatment of choice for other benign conditions, such as recurrent tonsillitis, sleep disordered breathing and OSA and therefore is a reasonable surgical approach for the treatment of tonsillar schwannoma.
There is no consensus on the post-operative follow-up interval in the reported cases, however there should be standard post-operative care and further follow-up at appropriate intervals to monitor for recurrence. We recommend standard post-operative follow-up at six to eight weeks and then re-review at six to twelve months to rule out recurrence of disease.
Limitations
The rarity of this disease is evident by the small number of cases reported in the literature since 1975. Thus, the evidence in this systematic review is comprised solely of case reports and hence the quality of evidence must be considered. The bias within included studies was low when assess with JBI checklist (see Appendix 1) as all the data required to complete this review was available in the published literature. Publication bias cannot be determined as meta-analysis or effect estimate could not be completed due to the small study population. Selection bias was avoided as all the available published cases of palatine tonsillar schwannoma were included in this review.
Possible limitations of this review arose from the variability in post-operative follow-up, which ranged from two weeks to eighteen months. There was no follow-up beyond eighteen months, which can potentially underestimate disease recurrence. There was also variability in demographic data reported for each patient, for example some cases reported patient ethnicity, smoking status, personal or family history of tumours etc., whilst others did not. This could potentially limit the generalisability of the results from this review.
This study is the first systematic review on palatine tonsillar schwannomas and can provide Otolaryngologists with valuable insights on how to investigate and manage this rare disease.
Conclusions
Tonsillar schwannoma is a rare, benign condition found mostly in the adult population. It can cause significant symptoms such as throat pain, dysphagia and odynophagia and can be alarming to a patient and their primary care physician. However, it is a relatively easy condition to treat, once investigated appropriately, with complete excision leading to negligible recurrence risk. This systematic review on tonsillar schwannomas summarises all known literature and provides a management algorithm which can be applied in clinical situations.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://www.theajo.com/article/view/10.21037/ajo-23-31/rc
Peer Review File: Available at https://www.theajo.com/article/view/10.21037/ajo-23-31/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://www.theajo.com/article/view/10.21037/ajo-23-31/coif). C.M. serves as an unpaid editorial board member of Australian Journal of Otolaryngology from November 2022 to October 2024. The other author has no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sharma P, Zaheer S, Goyal S, et al. Clinicopathological analysis of extracranial head and neck schwannoma: A case series. J Cancer Res Ther 2019;15:659-64. [Crossref] [PubMed]
- Tulli M, Bondi S, Smart CE, et al. Diagnosis and Treatment of Laryngeal Schwannoma: A Systematic Review. Otolaryngol Head Neck Surg 2018;158:222-31. [Crossref] [PubMed]
- Belakhoua SM, Rodriguez FJ. Diagnostic Pathology of Tumors of Peripheral Nerve. Neurosurgery 2021;88:443-56. [Crossref] [PubMed]
- Kocharyan AH, Briggs S, Cosetti MK, et al. Atypical Schwannoma: A 10-year experience. Am J Otolaryngol 2020;41:102309. [Crossref] [PubMed]
- Langner E, Del Negro A, Akashi HK, et al. Schwannomas in the head and neck: retrospective analysis of 21 patients and review of the literature. Sao Paulo Med J 2007;125:220-2. [Crossref] [PubMed]
- Boujguenna I, Ousehal H, Zaroual A, et al. A tonsillar location of a malignant schwannoma: a case report. Diagn Pathol 2022;17:48. [Crossref] [PubMed]
- Lee BJ, Wang SG, Lee JC, et al. Schwannoma of the tonsil. Ear Nose Throat J 2007;86:354-5. [Crossref] [PubMed]
- Anil HT, Gowda BV, Lakshmi S, et al. Schwannoma of the palatine tonsil. J Laryngol Otol 2005;119:570-2. [Crossref] [PubMed]
- Naik SD, Agrawal S. Neurilemmoma of tonsil. J Indian Med Assoc 1975;65:17-8. [PubMed]
- Khanal P, Shrestha A. Kimura's Disease: A Rare Cause of Unilateral Tonsillar Enlargement. Case Rep Otolaryngol 2021;2021:8815317. [Crossref] [PubMed]
- Ji H, Ulualp SO, Sengupta A. A rare cause of tonsil mass in a child: Lymphoid polyp. SAGE Open Med Case Rep 2017;5:2050313X16688832.
- Hay C, Kozielski R, Behar P. A Young Man With Enlarging Unilateral Tonsil Mass. JAMA Otolaryngol Head Neck Surg 2017;143:309-10. [Crossref] [PubMed]
- Ma LL, Wang YY, Yang ZH, et al. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: what are they and which is better? Mil Med Res 2020;7:7. [Crossref] [PubMed]
- Bildirici K, Cakli H, Keçik C, et al. Schwannoma (neurilemmoma) of the palatine tonsil. Otolaryngol Head Neck Surg 2002;126:693-4. [Crossref] [PubMed]
- Chaudhary N, Gupta D, Natesh V. Schwannoma of the palatine tonsil. Ear Nose Throat J 2011;90:E7-9. [Crossref] [PubMed]
- Goto Y, Iguchi H, Fujioka T, et al. Schwannoma of the palatine tonsil. Medical Journal of Minami Osaka Hospital 2012;59:75-8.
- Lall GS, Walsh RM, Rowlands DC, et al. Schwannoma (neurilemmoma) of the tonsil. J Laryngol Otol 1999;113:585-6. [Crossref] [PubMed]
- Pham TA, Zhao Y, Sigston E. Schwannoma of the Palatine Tonsil: A Rare Entity in an Eight Year Old Girl. J Clin Exp Oncol 2013;2:2. [Crossref]
- Piplani S, Manjari M, Sarin V, et al. Neurilemmoma Masquerading as Tonsillitis: A Case Report. Journal of Clinical and Diagnostic Research 2011;5:1092-4.
- Ruan LX, Zhou SH, Wang SQ. Palatine tonsil schwannoma: correlation between clinicopathology and computed tomography features. J Int Med Res 2008;36:1140-7. [Crossref] [PubMed]
- Datta PG, Akhtar N, Naha A, et al. Schwannoma of Tonsil. Bangladesh Med Res Counc Bull 2020;46:142-3. [Crossref]
- Joseph JA, Jaberoo MC, Sandison A, et al. Benign schwannoma of the tonsil. BMJ Case Reports; London; 2010. doi:
10.1136/bcr.02.2010.2707 .10.1136/bcr.02.2010.2707 - Li J, Wang Q, Zhang M, et al. Malignant Transformation in Vestibular Schwannoma: Clinical Study With Survival Analysis. Front Oncol 2021;11:655260. [Crossref] [PubMed]
- Håvik AL, Bruland O, Miletic H, et al. Genetic alterations associated with malignant transformation of sporadic vestibular schwannoma. Acta Neurochir (Wien) 2022;164:343-52. [Crossref] [PubMed]
- Cohen LM, Schwartz AM, Rockoff SD. Benign schwannomas: pathologic basis for CT inhomogeneities. AJR Am J Roentgenol 1986;147:141-3. [Crossref] [PubMed]
- Geltzeiler M, Doerfler S, Turner M, et al. Transoral robotic surgery for management of cervical unknown primary squamous cell carcinoma: Updates on efficacy, surgical technique and margin status. Oral Oncol 2017;66:9-13. [Crossref] [PubMed]
- Weinstein GS, O'Malley BW Jr, Snyder W, et al. Transoral robotic surgery: radical tonsillectomy. Arch Otolaryngol Head Neck Surg 2007;133:1220-6. [Crossref] [PubMed]
- Yasumatsu R, Nakashima T, Miyazaki R, et al. Diagnosis and management of extracranial head and neck schwannomas: a review of 27 cases. Int J Otolaryngol 2013;2013:973045. [Crossref] [PubMed]
- Trinidade A, Philpott CM. Bilateral glossopharyngeal nerve palsy following tonsillectomy: a very rare and difficult complication of a common procedure. J Laryngol Otol 2015;129:392-4. [Crossref] [PubMed]
Cite this article as: Kumar SA, Meller C. Contemporary management of tonsillar schwannoma—a systematic review. Aust J Otolaryngol 2023;6:28.