Impact of coronavirus disease 2019 (COVID-19) on Ear, Nose and Throat (ENT) surgery waitlists in regional centres
Introduction
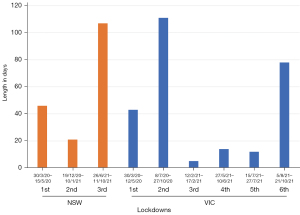
Otorhinolaryngology, Head and Neck (ORLHN) [Ear, Nose and Throat (ENT)] surgeons in regional Australia face a wide array of challenges when delivering healthcare to their patients (1), but the arrival of severe acute respiratory syndrome-related coronavirus 2 (SARS-CoV-2) [coronavirus disease 2019 (COVID-19)] saw many new hurdles. These included the additional strain of restricted elective surgery during the first wave of the pandemic. This was a coordinated response to ensure bed availability for predicted COVID-19 patients. The Australian Federal Government implemented a country-wide shutdown of all non-urgent elective operations from 25th March 2020, allowing only Category 1 and urgent Category 2 procedures to go ahead. All Category 2 and some Category 3 cases were allowed to resume from 27th April 2020, and by early May there were no country-wide restrictions on elective operating. There were subsequent periods in 2020 and 2021 of restricted access in states more severely affected by the pandemic (2) (Figure 1). Shutdowns were also instigated to facilitate access to personal protective equipment (PPE) for healthcare workers (HCWs), the supply of which was coming from overseas. Had standard operating lists continued, there were local concerns that HCWs would not have enough PPE available for standard consumption at higher protection levels. It also allowed time for vaccinations to be developed and to allow these vaccinations to be provided to all members of the community and health work force.
Research has evaluated the effect of COVID-19 on emergency and elective surgery in various major centres around the globe, including transplant waiting lists in the Netherlands (3), Orthopaedic surgeries in the UK (4,5) and Paediatric ENT services in the USA and South Africa (6,7). All previous studies have been focused on metropolitan centres. This study is the first to evaluate the impact of COVID-19 on ENT surgery waitlists in Australian regional centres where total COVID-19 case numbers were low, but despite this, elective surgery was still significantly disrupted. It is also the first study to analyse the effect of COVID-19 on surgical waitlist across different priority categories.
Categorisation of surgical priority is a longstanding practice in the Australian public healthcare system, ensuring that operations are scheduled based on clinical need as well as time spent on waiting lists. Category 1 is defined as urgent elective, Category 2 is semi-urgent elective, and Category 3 is non-urgent elective (8) (Table 1). All surgical disciplines have a general agreed list of which cases fall into each category.
Table 1
| Priority category | Time frame | Definition |
|---|---|---|
| Category 1 | 30 days | Urgent elective, with admission within 30 days desirable for a condition that has the potential to deteriorate quickly to the point that it may become an emergency |
| Category 2 | 90 days | Semi-urgent elective, with admission within 90 days desirable for a condition causing some pain, dysfunction or disability but which is not likely to deteriorate quickly or become an emergency |
| Category 3 | 365 days | Non-urgent elective, with admission at some time in the next 365 days acceptable for a condition causing minimal or no pain, dysfunction or disability, which is unlikely to deteriorate quickly and which does not have the potential to become an emergency |
Dubbo Health Service (DHS) and Albury Wodonga Health (AWH) are busy regional centres, with catchment areas of 150,000 and 250,000 people respectively. Both sites provide acute ENT services to the regions with typically 2–3 elective operating lists per week. DHS is a single campus hospital located in Dubbo in the Central West region of NSW and is administered by NSW Health. AWH is a multi-campus health service located across the border towns of Albury in NSW and Wodonga in Vic and is administered by the Victorian Department of Health. Both sites service large geographical areas (Figure 2). The sites were selected for analysis due to their large catchments and similar demographics, as well as their key difference being that AWH as a border town serves patients from two states while DHS only services NSW residents.
This study aims to evaluate and quantify the effect of elective operating shutdowns due to COVID-19 on the average time spent on ENT waitlists in regional areas, as well as the likelihood of breaching recommended waiting times. We hope to use this information as well as recommendations from the literature to prevent further unnecessary surgery shutdowns in the event of subsequent waves of the COVID-19 pandemic. We present the following article in accordance with the STROBE reporting checklist (available at https://ajo.amegroups.com/article/view/10.21037/ajo-22-1/rc).
Methods
A retrospective audit of elective ENT surgery waitlist times was performed at two regional centres in Australia—DHS in Dubbo NSW, and AWH in Albury NSW and Wodonga Victoria. Anonymised data was collected from a 2-year time period between 01/03/2019 and 28/02/2021, with the first 12 months (year 2019) considered pre-COVID and the second 12 months (year 2020) COVID affected. Waitlist data was grouped by the priority category assigned to elective surgery types, being Category 1, Category 2 and Category 3. Data was also separated into 3-month quarters, named Q1 through Q8 (Table 2). Waiting times were calculated as the number of days from the date of placement on waiting list until the day of procedure. Emergency surgeries were not included in the data collection.
Table 2
| Location and category | Number of cases | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2019 | 2020 | ||||||||||
| Q1 | Q2 | Q3 | Q4 | Total | Q5 | Q6 | Q7 | Q8 | Total | ||
| Albury (% change) | 246 | 281 | 302 | 254 | 1,083 | 80 (−67.50) | 174 (−38.10) | 203 (−32.80) | 193 (−24.00) | 650 (−40.00) | |
| Category 1 | 46 | 53 | 46 | 51 | 196 | 29 (−37.00) | 48 (−9.40) | 45 (−2.20) | 48 (−5.90) | 170 (−13.30) | |
| Category 2 | 110 | 128 | 138 | 114 | 490 | 32 (−70.90) | 74 (−42.20) | 111 (−19.60) | 74 (−35.10) | 291 (−40.60) | |
| Category 3 | 90 | 100 | 118 | 89 | 397 | 19 (−78.90) | 52 (−48.00) | 47 (−60.20) | 71 (−20.20) | 189 (−52.40) | |
| Dubbo (% change) | 159 | 161 | 117 | 127 | 564 | 86 (−45.90) | 153 (−5.00) | 176 (50.40) | 200 (57.50) | 615 (9.00) | |
| Category 1 | 12 | 12 | 20 | 22 | 66 | 9 (−25.00) | 25 (108.30) | 23 (15.00) | 17 (−22.70) | 74 (12.10) | |
| Category 2 | 35 | 35 | 21 | 34 | 125 | 38 (8.60) | 31 (−11.40) | 53 (152.40) | 40 (17.60) | 162 (29.60) | |
| Category 3 | 112 | 114 | 76 | 71 | 373 | 39 (−65.20) | 97 (−14.90) | 100 (31.60) | 143 (101.40) | 379 (1.60) | |
| Quarter dates | 1/3/19–31/5/19 | 1/6/19–31/8/19 | 1/9/19–30/11/19 | 1/12/19–29/2/20 | 1/3/20–31/5/20 | 1/6/20–31/8/20 | 1/9/20–30/11/20 | 1/12/20–28/2/21 | |||
Q, quarter.
Statistical analysis
Mean quarterly waiting times were calculated for each category within each time period. Mean waiting times for corresponding time periods (i.e., quarter 1 vs. quarter 4) were compared as well as year 2019 vs. 2020 as a whole, using t-test for independent samples to calculate statistical significance. Number of cases to have breached the waiting list category recommendations were recorded, and percentages of cases breached per period were calculated for each category. Proportions of breached cases from corresponding time periods were analysed using chi-squared testing to calculate statistical significance. Statistical analysis was performed using Microsoft Excel software.
Results
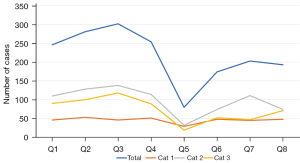
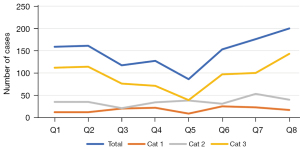
A total of 2,915 operations were recorded across both sites over the 2-year period, case numbers for both sites is included in Table 2. A total of 1,083 operative cases were performed at Albury in 2019, which decreased by 40% to 650 cases in 2020. At Dubbo, 564 operations took place in 2019, increasing by 9% to 618 cases in 2020. For the March–May quarter (which corresponded to nationwide elective surgery shutdowns in 2020), the number of cases in 2020 compared to 2019 fell by 67.5% at Albury and 45.9% at Dubbo, with the most significant decrease at both sites being for Category 3—falling by 78.9% in Albury and 65.2% in Dubbo. There were no periods at Albury where the number of cases of any category increased in 2020 compared to 2019 (Figure 3), however this did occur at Dubbo during the second half of the year 2020 (Figure 4).
Mean waitlist time
Albury
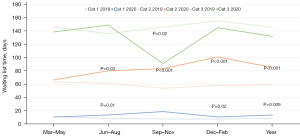
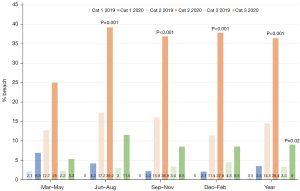
Mean waitlist times for Albury are presented in Figure 5. Annual mean waitlist time increased significantly for Category 1 (+59.5%, P=0.01) and Category 2 (+44.2%, P<0.001) for the year 2020 but decreased for Category 3 cases (−9.4%, not significant). For individual quarters, there were statistically significant increases in mean waitlist time between 2019 and 2020 for the June–August and December–February periods for Category 1 and the June–August, September–November and December–February periods for Category 2. There was a statistically significant decrease in the mean waitlist time between 2019 and 2020 for the September–November period for Category 3.
Dubbo
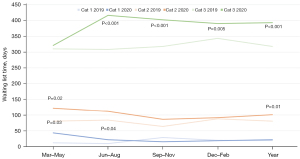
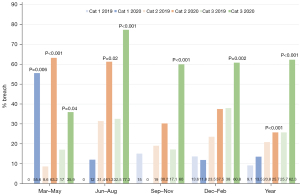
Mean waitlist times for Dubbo are presented in Figure 6. Annual mean waitlist time increased for Category 1 (+14.4%, not significant), and increased significantly for Category 2 (+25.1%, P=0.01) and Category 3 (+23.6%, P<0.001). For individual quarters, there were statistically significant increases in mean waitlist time between 2019 and 2020 for the March–May and June–August periods for Category 1, the March–May period for Category 2 and the June–August, September–November and December–February periods for Category 3. There were no statistically significant decreases in mean waiting time in any periods across any categories at Dubbo between 2019 and 2020.
Percentage of cases breaching recommended waiting time
Albury
The percentage of cases that breached the recommended waitlist time in Albury are presented Figure 7. Albury Category 2 cases breached waiting list recommendations 14.5% of the time in 2019 compared to 36.4% in 2020 (P<0.001), and Category 3 cases breached 3.3% in 2019 compared to 9% in 2020 (P=0.02). Category 1 data showed an increase in the proportion of cases breaching recommended 30 days waiting time, however this was not significant. For individual quarters at Albury, there were statistically significant increases in the percentage of breached cases between 2019 and 2020 for the June–August, September–November and December–February periods for Category 2. There were no statistically significant decreases in the likelihood of cases breaching waitlist recommendation in any periods across any categories at Albury between 2019 and 2020.
Dubbo
The percentage of cases that breached the recommended waitlist time in Dubbo are presented Figure 8. Dubbo Category 2 cases breached 20.8% in 2019 compared to 25.7% in 2020 (P<0.001) and Category 3 cases breaches 25.7% in 2019 compared to 62.3% in 2020 (P<0.001). Category 1 data showed an increase in the proportion of cases breaching recommended 30 days waiting time, however this was not significant. For individual quarters at Dubbo, there were statistically significant increases in the percentage of breached cases between 2019 and 2020 for the March–May period for Category 1, the March–May and June–August periods for Category 2 and all four periods for Category 3. There were no statistically significant decreases in the likelihood of cases breaching waitlist recommendation in any periods across any categories at Dubbo between 2019 and 2020.
Discussion
As demonstrated by our research, COVID-19 has had a considerable impact on both waiting times and likelihood of breaching waitlist recommendations for elective ENT surgery in regional centres. There is strong evidence to suggest that COVID-19 shutdowns lead to an increase in the likelihood of Category 2 and 3 cases breaching recommended waitlist times in Albury and Dubbo between 2019 and 2020. There was also a significant increase observed for the percentage of Category 1 cases breaching at Dubbo during the March–May quarter of 2020 compared to 2019, despite these cases being allowed to go ahead during the initial shutdown of non-urgent elective operating. This is thought to be due to the hesitancy of patients in accessing services at Dubbo Hospital during this initial wave of the COVID-19 pandemic with publicised confirmed cases being admitted to the service. Thankfully this same phenomenon was not observed across annual figures or other quarters for Category 1 cases at either site.
The lockdown period for the first wave in Australia may have only lasted for approximately one month in NSW, but this study shows that the effects on an already strained system have persisted for close to 12 months. Data from the Australian Institute of Health and Wellbeing (AIHW) showed that ENT surgery was severely impacted by COVID-19 in terms of the total number of admissions, with the figures for the 2019–2020 financial year falling 15.3% compared to 2018–2019 (8). This may be explained by a large proportion (up to 49% according to AIWH data) of ENT operations falling into Category 3 priority, resulting in suspension of a disproportionate number of cases compared to other specialties. Some of the most significant impacts were felt during each location’s corresponding lockdown period (Figure 1).
AWH faced additional challenges during the first wave of the COVID-19 pandemic. Due to its border location, the catchment area covers constituents from both NSW and Victoria but is administered by the Victorian Department of Health. Consequently, the health service was subject to restrictions as per other healthcare centres in Victoria despite being located in NSW. Victoria’s capital Melbourne was subject to 112 days of lockdown, one of the longest in the world at the time, and NSW-Victoria border restrictions were in place from 7th July 2020 until 23rd November 2020. This resulted in many patients not travelling for healthcare despite being allowed to do so. In addition, many NSW residents were unable to access necessary surgical procedures due to government restrictions on certain NSW Local government areas imposed by a health service being governed from a neighbouring state. Restrictions also resulted in halting of elective operating across a whole state, despite only one main metropolitan region being affected. This was despite lower case numbers per capita in less densely populated rural and regional towns.
According to the results of this study, the number of operative cases undertaken does not correlate to the time spent on waiting list, nor the likelihood of breaching the waitlist limit. The number of cases at Dubbo increased from June 2020 onwards, with an overall 9% increase in operations in the year 2020 compared to 2019. This increase in operative cases overall at Dubbo can be attributed to the aggressive waitlist reduction process that occurred from September 2020 until the end of February 2021. This reduced the impact of COVID-19 lockdown on waitlist times and the likelihood of breach. However, this intervention was only possible at Dubbo due to the coincidental availability of a consultant surgeon, theatre time and inpatient hospital beds, and was not possible at Albury due lack of inpatient beds and access to theatres. Interventions such as this should not be relied upon solely as a means of mitigating the impact of COVID-19 or other external factors on surgical waiting lists.
The issue of consultant availability in regional towns is a longstanding issue within Australia. The majority of the population lives in coastal capital cities and there is a higher number of specialists per capita compared to rural and regional centres (1). Dubbo and Albury are each serviced by two local ENT surgeons who are responsible for the ENT needs of 150,000 and 250,000 people respectively. This equates to one surgeon per 75,000 population in Dubbo, and one surgeon per 125,000 population in Albury. In 2016, 460 ENT specialists were registered to practice in Australia (9), serving a population of 24 million people and providing one surgeon per 52,000 population. 34.5% of these surgeons practiced in NSW (one surgeon per 47,000 population) and 25% in Victoria (one surgeon per 51,500 population). According to the Australian Society of Otolaryngology, Head and Neck Surgery (ASOHNS), the governing body for ENT specialists in Australia, for the safe provision of ENT services to the community one surgeon per 58,000 population is recommended (10). While Dubbo comes closer to this target, surgeons in Albury have close to triple the recommended catchment population to service. Recruitment of new surgeons to rural centres is difficult due to many factors, including the majority of training centres being metropolitan based (leading to higher retention of trainees as consultants), a fear of becoming professionally isolated, fear of being isolated from family based in cities and disincentivising of permanent positions when short term locum roles provide better renumeration (1,11). Fly-in, fly-out (FIFO) or Outreach providers may provide a temporising solution to support local surgeons by reducing the waitlist load as well as providing complex medical care (12), however they are less likely to be able to provide aftercare or manage complications, and should be utilised only after consultation with local teams in regional centres.
Surge planning for future waves of the pandemic has been undertaken at rural and metropolitan centres alike, however there are some issues surrounding this which are unique to rural surgeons. As above, rural centres are impacted by workforce shortage of consultant surgeons which leads to increased pressure on the remaining surgeon if the other is required to isolate due to COVID-19, a phenomenon not felt in metropolitan centres due to the proximity of other surgeons and local health districts (LHD). Redeployment of junior medical officers including surgical registrars occurred at DHS during the first wave of the pandemic in 2020, and as a result of there being only one ENT registrar this led to a decrease in the availability of prompt inpatient ENT reviews and emergency management. When consultants were contacted for inpatient reviews directly, special care was required to triage these reviews to reduce unnecessary exposure to COVID-19 given the consequences on the other consultant if one were to become infected. Recommendations have subsequently been put in place for future surge planning to not redeploy sole subspecialty registrars at DHS. At AWH, decisions were made early during the first wave to not allow redeployment of the ENT registrar, and for the two ENT surgeons to not meet face-to-face to ensure both were not exposed simultaneously during COVID-19 surges.
The impacts of lockdowns on both the diagnosis of ENT conditions as well as treatment and outcomes are an area requiring further research. Patients with ENT conditions faced issues getting in person appointments with their general practitioners (GPs) during the pandemic due to upper respiratory tract symptoms disallowing them entry to practices without a negative COVID-19 swab. These tests are harder to access in regional and rural locations, with patients often having to travel over an hour to a testing site. Furthermore, delays in turnaround of COVID-19 viral polymerase chain reaction (PCR) swab results in the early stages of testing created further impacts. This subsequently caused a reduction in the number of patients referred to ENT specialists for definitive management of their conditions (13). This improved when federal government funding for telehealth reviews was implemented. However, considering the importance of a thorough physical examination of the ENT system which is limited significantly on telehealth, there is the possibility that patients were not accurately referred even with GP telehealth consultations. The Albury service continued to see patients face-to-face throughout the whole pandemic with only an initial 3–4-week period (May–June 2020) when telehealth was used to triage all patients prior to a face-to-face consultation. Patients in Dubbo were unable to access in-person consultations for 2-month period from May to July 2020. Telehealth was felt to have a significant impact on diagnosis and management of head and neck cancers, hence the decision to continue to see patients in person to ensure sinister pathology was not missed (14). Patient attitudes towards COVID-19 have impacted on their presentation to healthcare providers (7,15). Many patients want to avoid possible exposure to the virus by travelling to doctors’ offices. This is especially true in regional centres where the nearest specialists are often hours away, and travel restrictions may be in place.
Nader et al. (16) investigated the impact of COVID-19 on Cardiac surgery in France during a 2-month period in 2020 compared to the same period in 2019, and found a 57% decrease in operations, as well as an increase in disease severity by the time of operation and increase in the likelihood of complications. Maringe et al. (17) assessed the impact of lockdowns in the UK on screening initiatives and subsequent survival of four major cancers—lung, breast, oesophageal and colorectal—and estimated that the years of life lost (YLL) due to delays in diagnosis and initiation of treatment to be more than 60,000. They also reported that the risk of death due to this delay in diagnosis is nearly as high as the risk of dying from COVID-19. While there are no formal screening programs in place in Australia for head and neck cancers, it is feared that the closure of consulting rooms and reduction in operating lists during lockdown could have had a negative impact on disease progression for these conditions and is an area warranting future research.
Many methods of managing waitlist times have been proposed, with research performed in this area well before the appearance of COVID-19. A systematic review by Rathnayake et al. (18) recommended a shift towards individual hospital or district-based strategies rather than system-wide approaches and developed a framework of common principles that were identified across each study. Categories included national and local considerations, horizontal equity (within individual disciplines) and vertical equity (across various disciplines), and incorporated clinical, socio-economic and moral considerations as well as patient reports, investigations, results and clinical judgment. Implementation of a strategy that incorporates these principles would be challenging, however likely to be more clinically accurate than the current method of assigning clinical priority which is often pre-determined by the operation type alone. Methods to reduce waiting times in the wake of lockdowns may include increasing operating list access such as was seen in Dubbo. Effectiveness of this approach is entirely dependent on availability of surgeon, theatre time and beds, and as previously stated has not prevented increases in waiting list times according to our study. Increasing operating lists may also require surgeons to reduce their time in consulting rooms, leading to loss of income as well as inadvertently increasing the waiting times for new patients to be reviewed in rooms. This in turn may contribute to delayed diagnosis and worsened disease progression, as seen in the UK (17), but will also falsely reduce the surgical waitlist times due to a decrease in the number of new patients being placed on these lists from the rooms. It should also be noted that disallowing new patients to be entered onto surgical waiting lists until the number is below a certain threshold is an unsafe and ineffective strategy, as it does not reduce the number of patients requiring intervention, and patients may be lost to follow-up prior to receiving their required intervention.
As the world now moves towards “living with COVID-19” and away from an eradication goal, so too should the lockdown strategies. During the first wave of COVID-19 in Australia very few cases were recorded in rural NSW and Victoria, yet Dubbo and Albury hospitals were still required to reduce non-urgent surgeries when they could have continued working and reduced already strained waiting lists. During the second wave of the pandemic in mid-2021, after the conclusion of the study period, Dubbo saw a large number of local cases which necessitated elective surgery shutdown in addition to stringent testing measures which still remain in place. However, the ability to increase capacity for elective surgical procedures in the recovery phase of the pandemic is not easy in an already under-resourced regional system, and the effects are expected to be felt for years to come. For future waves or exposures, more location specific lockdown and testing approaches should be implemented to reduce unnecessary strain in areas that are deemed low risk. Surgery should only be curtailed when a set agreed state- or nation-wide disease threshold is reached, especially regionally where disease spread is less likely and resources are stretched.
Regional patients are known to present later with worse disease, miss more work and have higher health care costs when compared to their metropolitan counterparts (1,12). During the pandemic, people from regional Australia have been shown to be very compliant with public health orders, with intra-regional travel restricted, testing and vaccination compliance rates very high and social distancing measures followed, equating to low regional disease rates. But despite these efforts, regional patients have paid a disproportionately high price during the COVID-19 pandemic.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://ajo.amegroups.com/article/view/10.21037/ajo-22-1/rc
Data Sharing Statement: Available at https://ajo.amegroups.com/article/view/10.21037/ajo-22-1/dss
Peer Review File: Available at https://ajo.amegroups.com/article/view/10.21037/ajo-22-1/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://ajo.amegroups.com/article/view/10.21037/ajo-22-1/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- National Ministry of Health. Rural Surgery Futures 2011-2021. 2012.
- Storen S, Corrigan N. COVID-19: a chronology of state and territory government announcements. Parliamentary Library, Parliament of Australia, 2021.
- de Vries APJ, Alwayn IPJ, Hoek RAS, et al. Immediate impact of COVID-19 on transplant activity in the Netherlands. Transpl Immunol 2020;61:101304. [Crossref] [PubMed]
- Clement ND, Oussedik S, Raza KI, et al. The rate of patient deferral and barriers to going forward with elective orthopaedic surgery during the COVID-19 pandemic. Bone Jt Open 2020;1:663-8. [Crossref] [PubMed]
- Chang J, Wignadasan W, Kontoghiorghe C, et al. Restarting elective orthopaedic services during the COVID-19 pandemic: Do patients want to have surgery? Bone Jt Open 2020;1:267-71. [Crossref] [PubMed]
- Bann DV, Patel VA, Saadi R, et al. Best Practice Recommendations for Pediatric Otolaryngology during the COVID-19 Pandemic. Otolaryngol Head Neck Surg 2020;162:783-94. [Crossref] [PubMed]
- McGuire JK, Fagan JJ, Peer S. Reintroduction of elective paediatric otolaryngology procedures in South Africa during the COVID-19 pandemic. S Afr Med J 2020;110:601-4. [Crossref] [PubMed]
- Australian Institute of Health and Welfare. My Hospitals update: Elective surgery waiting times 2019–20. 2021.
- Department of Health. Otolaryngology 2016 Factsheet. Australian Government, 2017.
- Royal Australasian College of Surgeons. Surgical Workforce Projection to 2025 (for Australia). 2011.
- McGrail M, O’Sullivan B, Russell D, et al. Solving Australia's rural medical workforce shortage. Centre for Research Excellence in Medical Workforce Dynamics. University of Melbourne, 2017.
- O'Sullivan BG, McGrail MR, Stoelwinder JU. Reasons why specialist doctors undertake rural outreach services: an Australian cross-sectional study. Hum Resour Health 2017;15:3. [Crossref] [PubMed]
- Scott A. The impact of COVID-19 on GPs and non-GP specialists in private practice. Melbourne Institute: Applied Economic & Social Research 2020;
- Wu V, Noel CW, Forner D, et al. Considerations for head and neck oncology practices during the coronavirus disease 2019 (COVID-19) pandemic: Wuhan and Toronto experience. Head Neck 2020;42:1202-8. [Crossref] [PubMed]
- Heward E, Rocke J, Kumar N, et al. Recurrent tonsillitis and parental perceptions of tonsillectomy during the COVID-19 pandemic. Int J Pediatr Otorhinolaryngol 2020;139:110463. [Crossref] [PubMed]
- Nader J, Anselmi A, Tomasi J, et al. Adult cardiac surgery during COVID-19 lockdown: Impact on activity and outcomes in a high-volume centre. Arch Cardiovasc Dis 2021;114:364-70. [Crossref] [PubMed]
- Maringe C, Spicer J, Morris M, et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol 2020;21:1023-34. [Crossref] [PubMed]
- Rathnayake D, Clarke M, Jayasinghe V. Patient prioritisation methods to shorten waiting times for elective surgery: A systematic review of how to improve access to surgery. PLoS One 2021;16:e0256578. [Crossref] [PubMed]
Cite this article as: Jaensch S, Tweddle E. Impact of coronavirus disease 2019 (COVID-19) on Ear, Nose and Throat (ENT) surgery waitlists in regional centres. Aust J Otolaryngol 2022;5:18.