
Laryngeal electromyography for vocal fold palsies—a modified technique in the Australian paediatric population
Introduction
Paediatric vocal fold paralysis (VFP) is an uncommon but important clinical entity as it leads to airway, speech, and swallowing dysfunction. Laryngeal electromyography (LEMG) in the paediatric population has been utilised as a tool for diagnosis and prognosis of this patient group. Its main function is in the assessment of patients with laryngeal motility disorders including unilateral or bilateral vocal cord immobility.
Currently there are no standardised method in performing paediatric LEMG. This leads to difficulty in interpreting and standardising LEMG. In Australia, we are also limited in the availability of the various lengths of electrodes. This may lead to challenges when performing LEMG during direct laryngoscopy and bronchoscopy (DLB) in a general anaesthetic setting, especially in a paediatric patient where the available space is limited.
The purpose of this paper is to present a method of LEMG which allows for ease of insertion of electromyography (EMG) electrode during a direct laryngoscopy procedure.
Laryngeal EMG technique
Inhalational anaesthesia in the operating theatre is used for the standard DLB. A monopolar ground electrode is placed onto the right shoulder. The patient is placed into suspension using the age appropriate Parsons laryngoscope. The DLB is performed with a 0 degree rigid endoscope (Hopkins® telescope, Karl Storz, Germany) and the cricoarytenoid joint (CAJ) is palpated to rule out fixation. Under direct endoscopic guidance the 50 mm disposable (Natus® Medical Incorporated, San Carlos, USA) concentric bipolar needle is inserted into the thyro-arytenoid and posterior cricoarytenoid. We found it challenging to insert the electrode due to length, as well as the large size of the belly of the handle. This issue is resolved by trimming the belly with a scalpel, and by inserting the wire of the electrode into a mixing cannula (Fairmont Medical Pty Limited, Victoria, Australia) and securing this with adhesive tape (Figure 1). The cannula provided increased length as well as rigidity, where the mid portion of the cannula was grasped free hand. The needle can then be easily advanced to the appropriate site. For the thyroarytenoid muscle the needle is inserted into mid portion. The recordings are taken (Keypoint® Focus Compact EMG/NCS/EP System, Dantec TM, Natus® Medial Incorporated, San Carlos, USA). For the posterior cricoarytenoid muscle the needle is inserted in the posterolateral aspect of the cricoid, inferior to the arytenoid cartilage and recordings are taken. This is repeated on both sides.

In our institution, the LEMG is done with a paediatric otolaryngologist who facilitate the insertion of the electrode into the appropriate site, a paediatric neurologist with training in electromyography, as well as a paediatric neurophysiologist. Examples of LEMG recordings can be seen in Figure 2 and Table 1.
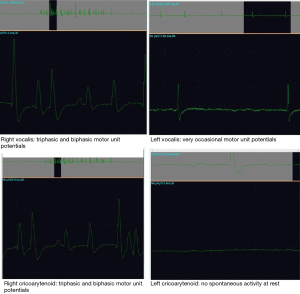
Table 1
| Muscle | Insertional activity | Spontaneous/rest | MUPs | Recruitment pattern |
|---|---|---|---|---|
| Right vocalis | Normal | Nil | Biphasic/triphasic normal | NA |
| Left vocalis | Reduced | Fibs+ PSW+ | Reduced | NA |
| Right cricoarytenoid | Normal | Nil | Biphasic/triphasic normal | NA |
| Left cricoarytenoid | No insertional activity tested 4 times | Nil | Very occasional | NA |
LEMG, laryngeal electromyography; MUP, motor unit potential; NA, not applicable; Fibs, fibrillations; PSW, positive sharp waves.
Discussion
Paediatric VFP is the second most common laryngeal anomaly following laryngomalacia (1). Idiopathic and iatrogenic aetiologies are most common (2). The recovery of VFP is unpredictable, but it is suggested that up to two third of patients with idiopathic VFP will recover, with delayed recovery up to the age of 11 years being observed (2). This creates significant challenges in providing counselling of parents of patients with paediatric VFP as well as providing guidance on when it would be optimal to intervene.
LEMG has been used in the paediatric population to provide diagnostic information and at times influence clinical decision making and treatment plans (1). Laryngeal EMG is used as an extension of clinical examination and not in isolation. On insertion of the needle into the laryngeal muscles we can get an idea of the insertional activity which will be reduced or lost in an atrophic muscle. If there are active denervation changes seen on the EMG it suggests damage to the nerve supply and helps in determining the stage of nerve damage and the degree of nerve damage. Procedures for reconstruction should take into consideration the degree of atrophy of the laryngeal muscles. CAJ fixation can be diagnosed in the setting of s normal LEMG activity in an immobile cord on flexible nasendoscopy. Intra-operative palpation of the CAJ is also diagnostic.
The EMG is most useful in unilateral vocal cord (VC) palsy as we can compare the waveforms with the unaffected side. However, it is important to consider serial LEMG in some cases.
In adults, the use of conventional LEMG is an office based procedure (3). The paediatric population presents specific challenges for LEMG. Firstly, the procedure is performed under general anaesthesia due to compliance. Secondly, the paediatric larynx is relatively small, making accurate placement of the monopolar electrode challenging, therefore modifications in the use of equipment may be required. Thirdly, LEMG equipment and LEMG trained neurologist are necessary in the theatre concurrently with the otolaryngologist, so that real time feedback is provided in terms of electrode placement, acoustic profile and electric activity.
In our practice, we utilise inhalation anaesthesia as it has been shown to be superior to total intravenous anaesthesia in an animal model, as it does not affect the quality of the LEMG and allows for DLB (4). Once the patient is settled in suspension laryngoscopy, we found that grasping the short length electrode with laryngeal grasper and inserting it into required sites was challenging. Therefore, we modified the equipment by securing it to a mixing cannula which can be adjusted in length and grasped at any point, or even used free hand in small infants, allowing for improved angles and easy insertion of the electrode into the necessary entry points. Finally, our LEMG equipment is portable, and this is mobilised into the theatre environment, and a neurophysiologist and LEMG neurologist are present concurrently during the procedure (Video 1).
It is not our practice to monitor the intercostals for the specific part of the respiratory cycle as it is currently not felt that this provides additional information. The patient is spontaneously breathing throughout the assessment and we aim to not alter the anaesthetic or take recordings as the patient emerges so as to not risk excessive movement causing displacement of the electrode needle and subsequent trauma to the vocal folds.
The current role in our unit is adjunct to other established procedures including diagnostic laryngotracheal bronchoscopy, amongst others. It also has a role to play to guide definitive management for instance in the setting of recurrent laryngeal nerve re-innervation, as well is a role in prognostication. Serial LEMG is performed to ensure there is no recovery over the observation period to guide discussion with parents.
Conclusions
LEMG is a useful technique for the assessment of patients with VCP. In the paediatric cohort there are some specific technical challenges. Here we present a modification for the electrode to allow for an improved ease and accuracy of insertion of the electrode.
Acknowledgments
The authors would like to acknowledge Christina Mitrovic: Neurophysiologist.
Funding: None.
Footnote
Peer Review File: Available at https://www.theajo.com/article/view/10.21037/ajo-21-11/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://www.theajo.com/article/view/10.21037/ajo-21-11/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Scott AR, Chong PS, Randolph GW, et al. Intraoperative laryngeal electromyography in children with vocal fold immobility: a simplified technique. Int J Pediatr Otorhinolaryngol 2008;72:31-40. [Crossref] [PubMed]
- Daya H, Hosni A, Bejar-Solar I, et al. Pediatric vocal fold paralysis: a long-term retrospective study. Arch Otolaryngol Head Neck Surg 2000;126:21-5. [Crossref] [PubMed]
- Woo P. Laryngeal electromyography is a cost-effective clinically useful tool in the evaluation of vocal fold function. Arch Otolaryngol Head Neck Surg 1998;124:472-5. [Crossref] [PubMed]
- Gazzaz M, Saini J, Pagliardini S, et al. Comparison of inhaled versus intravenous anesthesia for laryngoscopy and laryngeal electromyography in a rat model. J Otolaryngol Head Neck Surg 2018;47:64. [Crossref] [PubMed]
Cite this article as: Esmaili A, Kava M, Ha JF. Laryngeal electromyography for vocal fold palsies—a modified technique in the Australian paediatric population. Aust J Otolaryngol 2022;5:10.


