Practice patterns in myringoplasty surgery among Australian surgeons
Introduction
Myringoplasty is a commonly performed procedure in otolaryngology. It is used to treat symptomatic perforations of the tympanic membrane. Despite the prevalence of this procedure, there is a lack of consensus on best practice and significant variation globally.
Most of the recent literature relates to outcomes and success rates of myringoplasties rather than the actual practices or variations between surgeons. Several recent articles from Europe and the UK looked specifically at different factors affecting outcomes, but again there was little focus on actual variations in practices (1-3). There is a significant amount of published international data regarding the effectiveness of the different factors such as approach, choice of graft material and length of stay, but a relative paucity on how often particular techniques have been used (4-10). This has the potential to affect uptake of new techniques, and adoption of evidenced based practice. For example, it is unknown if the recent increase in the popularity of endoscopic ear surgery has actually translated to surgical practice.
In the 2018–2019 period 1,715 myringoplasties were performed in Australian hospitals (11). Myringoplasty surgery is considered a core surgical skill among Australian otolaryngologists as well as in many other countries. There are standardised assessments and compulsory audits of a trainee’s performance in this skill. Despite this, there remains no current universally established protocol for performing this procedure, likely due to the fact that there is more than one acceptable way of performing the surgery.
Australia is a geographically large and ethnically diverse country. We hypothesised that there was likely to be considerable practice variation among surgeons given the heterogeneous nature of conditions in which myringoplasties were performed. Australian otolaryngologists practice includes metropolitan areas, as well as rural and remote communities. Many surgeons operate on both adult and pediatric patients. This is a reflection of the fact that myringoplasty surgery is usually within the scope of all Otolaryngologists and is not restricted to sub-speciality trained otologists. We also hypothesise that the high rate of chronic suppurative otitis media amongst Indigenous Australians also has the potential to affect myringoplasty surgical techniques in these group of patients.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/ajo-19-5).
Methods
A cross-sectional study was conducted in order to obtain a snapshot of myringoplasty practices across Australia. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Department of Health Western Australia Human Research Ethics Committee - South Metropolitan Heath Service ethics board (Application No. CC00958) and informed consent was taken from all individual participants.
An anonymous 82-question online survey was designed by the authors. It included a mix of multiple choice, preferential and open questions, focusing on indications for surgery, antibiotic use, preferences for approach, graft type and material, and variations used in different patient demographics. Respondents were able to choose more than one answer to open ended questions.
A link to the questionnaire was electronically distributed to all 334 currently practicing otolaryngologists registered as full members of the Australian Society of Otolaryngology, Head and Neck Surgeons (ASOHNS). Results were collected via Survey Monkey (Palo Alto, California, USA) software.
To control for possible confounders, separate subgroup comparisons were undertaken considering the surgeon’s area of subspecialisation, patient demographics and perforation characteristics.
Results
Responses were collected from 124 out of 334 surgeons registered with ASOHNs representing 37% of all currently practising ENT surgeons in Australia. The survey was sent by the ASOHNS secretariat to its respective members and was open for a 3-month period.
Demographics
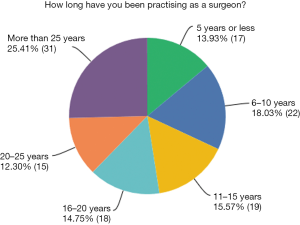
Just over one quarter of respondents had over 25 years’ experience as a surgeon, and 13.9% had 5 years or less (Figure 1). Many respondents had specialised in multiple areas. Of the surgeons surveyed, 32.8% of respondents identified as having subspecialised in otology, 38.5% in general ENT, 30.3% in paediatric ENT, 27.9% in rhinology, 9.8% in laryngology and 7.4% in facial plastics.
The majority of surgeons practiced in metropolitan areas but also did some rural work. However, over 70% performed myringoplasties solely in metropolitan hospitals whilst only 9.8% reported working in rural areas alone. Most otologists and general ENT surgeons believed myringoplasty could be performed by all ENT surgeons and should not just be limited to subspecialists (84.6% and 92.7% respectively).
Patient selection
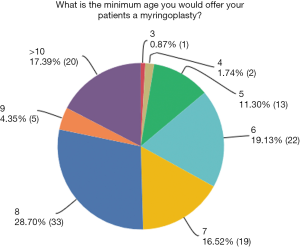
The median youngest patient age at which a surgeon would perform a myringoplasty was 8 years (28.7%) (Figure 2). The most common reasons given for this related to better eustachian tube function (86.4%), followed by better initial success rates (48.7%) and then long term success rates (43.4%).
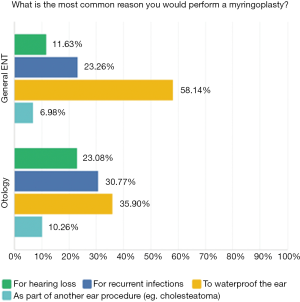
Waterproofing the ear was the most common indication for performing myringoplasty (45.2%), followed by recurrent infections (28.7%) then hearing loss (19.13%); 53.5% of respondents said they would offer myringoplasty to patients with normal hearing if they wanted to waterproof ear or prevent recurrent discharge. Fewer otologists performed myringoplasty with the primary goal of waterproofing the ear, compared to general ENT surgeons (38.5% vs. 50.0%). When viewed as a subgroup, the most common reasons for performing myringoplasty amongst sub-speciality trained otologists was also to waterproof the ear, follow by preventing recurrent infections (Figure 3).
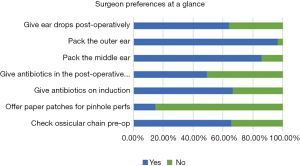
The majority of surgeons stated that the minimum hearing loss for patient to be considered suitable for a myringoplasty should be ≤20 dB (60.7%), and one third responded it should be in the 21–30 dB range (33.9%). Almost two thirds of surgeons routinely checked the status of ossicular chain with one third not routinely doing so. Of those who did not do so routinely, most would if the hearing level fell into the 21–50 dB range. Surprisingly, 45.1% of surgeons would offer surgery for hearing loss for an air bone gap of 11–20 dB and 31.0% would for one of 21–30 dB.
When asked about how long they would observe an acute perforation for, 41.6% surgeons reported waiting 3–4 months before offering a myringoplasty, with 40.7% preferring to wait over 5 months. Only 14.9% of surgeons would offer a paper patch for an acute perforation. The most common indications for the use of paper patches were for pinhole perforations, in patients unable to tolerate general anaesthetic, or at a patient’s request.
Surgical preferences
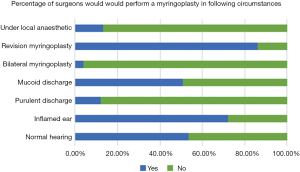
All of respondents routinely operated under a general anaesthetic; 13.1% said they also occasionally operated under local anaesthesia, a practice that was more common amongst otologists compared to general ENT surgeons (23.1% vs. 7.0%). Only 3.9% of surgeons reported performing bilateral simultaneous myringoplasties, making this an uncommon practice (Figure 4).
There was significant variation in use and choice of antibiotics and ear drops. Two thirds of respondents gave antibiotics on induction, usually cefazolin. This practice was also more common among otologists compared to general ENT surgeons (82.1% vs. 52.1%) (Figure 5).
About half (49.1%) of surgeons gave antibiotics post-operatively (Figure 5). The most common regimes were either oral cephalexin or amoxicillin/clavulanic acid for an average duration of 5 days; 64.0% prescribed post-operative ear drops. Ciprofloxacin based solutions were most common type of ear drops used, although the duration of prescription varied widely from 5 days to 6 weeks.
The majority of surgeons used ear packing, with 86.0% routinely using middle ear packing and 96.5% outer ear packing (Figure 5). Gelfoam was the most common type of packing for both. The duration of packing varied considerably, but the average was for 2 weeks.
Adults
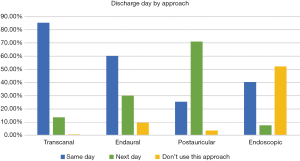
The majority of surgeons performed same day transcanal, endaural and endoscopic surgeries. Most respondents kept patients who had post-auricular approaches for a single overnight stay.
In adults, temporalis fascia (60.7%) was the most popular choice of graft material, followed by tragal perichondrium (29.3%) then tragal cartilage (8.0%). Only one person used fat as their first choice of graft material, indicating its lack of popularity. The most common combination of materials used was cartilage and perichondrium. Other less frequently used graft materials included Biodesign, conchal cartilage, gelfoam, pericranium, periosteum, fibrous tissue and tissue patches. No respondents specified where their tissue patches were harvested from.
A total of 94.6% preferred using underlay grafts in adults. A small minority used inlay grafts (5.1%) as their first preference, and 2.5% used overlay as their first choice. The transcanal route was the most popular approach (49.0%), followed by endaural (31.4%), post-auricular (21.7%), then endoscopic approaches (8.1%) (Figure 6).
Children
Temporalis fascia (51.4%) was again the most popular choice of graft material in children, followed by tragal perichondrium (27.1%), tragal cartilage (11.8%) then fat (10.5%) This was the same order of preference as for adults. Cartilage and perichondrium was also the most commonly used graft combination in children. Underlay grafts were preferred by the majority of surgeons when operating on children (89.6%). However, Inlay grafts were twice as likely to be preferred in children compared to adults (11.4% vs. 5.1%, P=0.001). As in adults, most surgeons preferred the transcanal approach (63.7%), followed by endaural (20.4%), postauricular (16.0%) and endoscopic (8.7%) approaches (Figure 6).
Rural vs. metropolitan areas
Most surgeons did not vary their practice when operating outside of metropolitan areas. Only 12.0% of respondents changed their approach if operating in a rural location, and 10.2% changed their choice of graft material.
Indigenous patients
In total, 21.3% of respondents changed their approach when operating on Indigenous patients. However, most differences in practice related to ear packing, rather than graft material, graft placement or approach. Of the surgeons who reported modifying other parts of their management for Indigenous patients: 3 only used dissolvable packing, 1 only used non-dissolvable packing, 2 left packing in for longer, and 2 sutured packing in place (Figure 6).
Perforation characteristics
Two thirds of respondents said the size of perforation affected their choice of graft material; 75.0% said it affected their choice of surgical approach, with post aural approaches being more popular for larger perforations, and transcanal approaches for smaller perforations; 73.3% also said it affected the success rate they would quote. Fat was more likely to be used for pinhole perforations and cartilage for small ones.
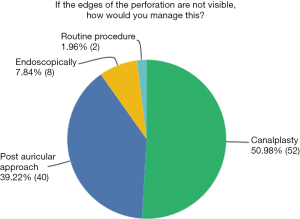
In total, 51.0% of surgeons routinely performed a canalplasty if the edges of perforation were not visible and 39.2% performed a postauricular approach in this situation. Among otologists 66.7% would routinely perform a canalplasty in this situation, compared to 48.5% of other ENT surgeons.
Only 2.0% of surgeons would perform their routine approach regardless of perforation visibility indicating that access is a key factor in determining approach (Figure 7). When filtered by surgeons whose first preference was an endoscopic approach there were no comments relating to canalplasty.
In total, 88.9% of surgeons preferred to use underlay grafts for subtotal perforations. Temporalis fascia was the most popular choice of graft materials for subtotal perforations (72.2%).
The postauricular approach was the most popular for anterior perforations (75.0%), and transcanal the most popular approach for posterior perforations (59.6%). Endaural approached were the second most favoured approached for both anterior and posterior perforations (30.2% and 47.9%). Endoscopic was the least favoured approach for both anterior and posterior perforations (17.7% and 13.8%) (Figure 6).
In total, 72.0% of surgeons would operate on an ear that was inflamed but only 11.9% would operate on an ear that was purulent; 51.0% would operate on an ear with mucoid discharge (Figure 4). The main reasons cited for operating on a non-dry ear was if patient was deemed unlikely to ever achieve a dry ear, or if they had travelled a long distance for their surgery.
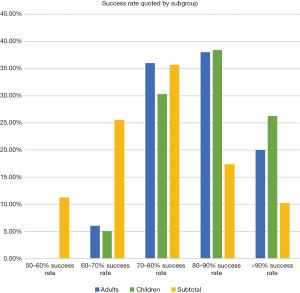
Success rates and follow up
Most surgeons quoted between a 70% to 90% success rate in both children and adults (Figure 8). This was slightly less for subtotal perforations, at 60% to 90%; 87.3% of respondents defined success as closure of perforation, 7.9% as a dry ear, and the remainder as an improved level of hearing.
In terms of post-operative instructions, over half of surgeons advised waiting 1 month before flying. However, a small minority allowed patients to fly immediately (6.9%). Two thirds allowed patients to get their ears wet within 2 months of surgery.
Revision surgery
In total, 86.3% of respondents performed revision myringoplasties, and the majority of those who did not referred to a colleague who subspecialised. The most commonly quoted success rate for revision surgery was between 60% to 80% (Figure 9). Only 40.2% of surgeons changed graft type for revisions, usually to a composite or either one containing perichondrium or cartilage.
Discussion
Our study appears to provide a good snapshot of myringoplasty practices amongst Australian surgeons. It supports the premise that it is a procedure not confined to specialist otologists and that this is an acceptable convention.
Waterproofing the ear is the most common indication for surgery and probably reflects the warm Australian summer climate and popularity of water-based recreational activities. The lack of consensus around hearing levels which would prompt surgery is also a likely reflection of the need to waterproof the ear being a greater consideration than hearing loss. Despite this, it is reassuring to know that the majority of surgeons assess the ossicular chain at the time of surgery. The reason for this is uncertain but may reflect conventional practice or the likely occurrence of concurrent ossicular pathology in the population.
The lack of paper patch or fat plugs as methods for myringoplasty are striking. This may reflect either unique practice patterns amongst Australian surgeons, the perceived lack of benefit of these techniques which may be real or otherwise, or the relatively small indication for these techniques. The relatively poor uptake of endoscopic myringoplasty in our cohort, typically considered an introductory procedure for aspiring endoscopic surgeons, is also notable. This has implications for proponents of endoscopic ear surgery who may wish to see greater adoption of this technique which has advantages over conventional open surgery (12). Endoscope use in ear surgery has the potential to reduce the morbidity of a larger postauricular scar or canalplasty, and thus also may reduce the need for an overnight stay with subsequent health cost benefits.
With regards to the use of graft material, fascial grafts remain the most popular and are inserted via an underlay technique. Newer materials, such as Biodesign (Cook Medical), are therefore more likely to be used as a substitute as it mimics fascia in its application. Two respondents also reported using gelfoam. No other biomaterials were reported by respondents. There seems to be a wide variability in practice with regards to the use of postoperative antibiotics. This may be an opportunity to develop guidelines to streamline the use of antibiotics particularly in the era of increasing antibiotic resistance. What is interesting is that the majority of surgeons would continue to operate in a less than optimal dry ear. This may be reflective of the conflicting evidence in the status of the ear being an important factor to improve outcomes (13). Further research is perhaps required to help guide and refine practice.
Myringoplasty is one of the most commonly performed otologic procedures. Despite this, consensus guidelines are lacking on the peri-, intra- and post-operative practices. Our thorough review of the literature revealed only 5 articles which related specifically to myringoplasty in Australia published in the last 15 years. Three were published prior to 2005 and focused specifically on success rates. The first focused on remote Indigenous Australia (14), the second was an audit of cases done at the Royal Victorian Eye and Ear Hospital (4), and the third was a case series looking at the myringoplasty success rate in Indigenous children (5). There was also an international meta-analysis led by a local Western Australian published in 2016, which examined factors affecting myringoplasty success, but it did not provide specifics about variations between surgeons or specific practices (6). The most recent article assessed the outcomes of myringoplasty in Indigenous adults (12). The significant lack of local myringoplasty literature is therefore an important knowledge gap that should be addressed, especially since it is an integral part of otolaryngology training in Australia. Several recent articles from Europe and the UK also looked at different factors affecting outcomes, but again there was little focus on actual variations in practices among surgeons (1-3). Additional specific searches were conducted to examine how long surgeons would forbid their patient from flying post-myringoplasty, and what ages they would consider suitable for myringoplasty candidates. Results for both these searches also focused on outcomes rather than variations in practices. However, 2 retrospective studies, which included both adults and children as young as 3, found no difference in graft healing rates in patients who flew within a week of surgery (15,16).
The authors are uncertain as to the reasons for the apparent lack of more widespread adoption of the endoscopic approach. The large proportion of myringoplasties being performed transcanal with the microscope does suggest that these cases have good exposure with this technique and potentially could have been done with the endoscope which is essentially a transcanal technique. This suggests that the reason for choosing a transcanal microscope technique over transcanal endoscopic technique is not due to a lack of exposure. These reasons may include lack exposure or training with the endoscopic approach, a lack of equipment, or a combination of these. This study was not specifically designed to survey the reason for a lack of adoption of endoscopic ear surgery techniques and perhaps future surveys may show a change in practice patterns over time as current registrars who are more likely to be exposed to endoscopic ear surgery in their training, graduate into consultant surgeons and adopt endoscopic techniques.
There were also several papers examining the effectiveness of the following practices, but limited detail on how often they were used in certain practice populations. Specific publications looked at general factors affecting success (7), endoscopic vs. microscopic approaches (8,9), different graft materials (10,15), whether different approaches can be done as day cases vs. overnight stays (16), and post-operative complication rates for different techniques (17). Whilst it appears that there are factors which can affect success, the homogeneity of approaches used in our population is probably reflective of real world practice patterns and different case mixes. In other words, it may be unreasonable to expect all myringoplasty cases in all patients to be the same. Our study also provides insight into the decision making processes of Otolaryngologists when faced with certain patient and disease factors. No articles looking specifically at surgeon’s preferences regarding age range for myringoplasty candidates were identified. However, many articles also looked at outcomes by age. One article concluded that children aged 4 years and younger have significantly worse outcomes compared with school age children (18). Another concluded that delaying surgery can cause permanent damage to the inner ear, and advocate early myringoplasty (19). Our study suggests that Australian surgeons practice broadly in line with these papers.
A key strength of this study is the relatively high response rate, capturing the current practices of over one third of Australia’s currently practising otolaryngology surgeons.
However, cross-sectional studies are not without limitations. While the average overall completion rate was excellent many respondents chose not to respond to the open ended questions. We believe this is in part due to the length of the survey and the fact that our study demographics are generally time poor. Whilst we did try to provide as much choice as possible for each question to capture the surgeon’s preference, multiple choice questions do create inherent bias by forcing a particular answer. Despite this, our results and their homogeneity appear to be in keeping with our local institutional practices and is therefore a fair representation of what most surgeons in Australia are likely to be practising on a day to day basis.
Our study is novel because it is the first study of which we are aware that addresses the current gap in knowledge regarding the wide variety of myringoplasty practices currently employed by otolaryngologists in Australia. It is hoped this data can be used as a baseline for comparison for future studies in other countries. We believe the variation in practice reflects the diversity in literature but also provides interesting insights into the lack or perceived lack of practical and applicable literature around certain aspects of myringoplasty surgery.
Conclusions
This is the first study looking at practice variation in myringoplasty surgery and demonstrates the diverse range of practice patterns among Australian surgeons. Development of evidence-based consensus guidelines may be useful in helping to refine the surgical treatment of tympanic membrane perforations.
Acknowledgments
The authors acknowledge the Australian Society of Otolaryngologists, Head and Neck Surgeon for helping to distribute this survey.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/ajo-19-5
Data Sharing Statement: Available at http://dx.doi.org/10.21037/ajo-19-5
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ajo-19-5). JK serves as an unpaid editorial board member of Australian Journal of Otolaryngology from Jan 2019 to Dec 2020. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Department of Health Western Australia Human Research Ethics Committee - South Metropolitan Heath Service ethics board (Application No. CC00958) and informed consent was taken from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ryan RM, Brown P, Cameron J, et al. Royal College of Surgeons comparative ENT audit 1990. Clin Otolaryngol Allied Sci 1993;18:541-6. [Crossref] [PubMed]
- Phillips JS, Yung M, Nunney I. Myringoplasty outcomes in the UK. J Laryngol Otol 2015;129:860-4. [Crossref] [PubMed]
- Preuss SF, Luers JC, Beutner D, et al. Results of a European survey on current controversies in otology. Otol Neurotol 2007;28:774-7. [Crossref] [PubMed]
- Brown C, Yi Q, McCarty DJ, Briggs RJ. The success rate following myringoplasty at the Royal Victorian Eye and Ear Hospital. Aust J Otolaryngol 2002;5:21.
- Mak D, MacKendrick A, Bulsara M, et al. Outcomes of myringoplasty in Australian Aboriginal children and factors associated with success: a prospective case series. Clin Otolaryngol Allied Sci 2004;29:606-11. [Crossref] [PubMed]
- Tan HE, Santa Maria P, Eikelboom R, et al. Type I Tympanoplasty Meta-analysis: A Single Variable Analysis of More Than 26 Thousand Adults and Children From 214 Studies. J Laryngol Otol 2016;130:S64-5. [Crossref]
- Carr SD, Strachan DR, Raine CH. Factors affecting myringoplasty success. J Laryngol Otol 2015;129:23. [Crossref] [PubMed]
- Huang TY, Ho KY, Wang LF, et al. A Comparative Study of Endoscopic and Microscopic Approach Type 1 Tympanoplasty for Simple Chronic Otitis Media. J Int Adv Otol 2016;12:28-31. [Crossref] [PubMed]
- Dündar R, Kulduk E, Soy FK, et al. Endoscopic versus microscopic approach to type 1 tympanoplasty in children. Int J Pediatr Otorhinolaryngol 2014;78:1084-9. [Crossref] [PubMed]
- Çatli T, Çelik Ç, Demir E, et al. Investigation of myringosclerosis development in different grafting materials after myringo-/tympanoplasty. Kulak Burun Bogaz Ihtis Derg 2015;25:65-9. [Crossref] [PubMed]
- Welfare AIoHa. Elective Surgery - 2018-2019 2020. Available online: www.aihw.gov.au
- Lakpathi G, Reddy LS. Comparative study of endoscope assisted myringoplasty and microscopic myringoplasty. Indian J Otolaryngol Head Neck Surg 2016;68:185-90. [Crossref] [PubMed]
- Soumya S, Hinton-Bayre A, Coates H, et al. Myringoplasty outcomes of Indigenous Australians in the West Kimberley region of Western Australia. Aust J Otolaryngol 2018;1:18. [Crossref]
- Mak D, MacKendrick A, Weeks S, et al. Middle-ear disease in remote Aboriginal Australia: a field assessment of surgical outcomes. J Laryngol Otol 2000;114:26-32. [Crossref] [PubMed]
- Khan MM, Parab S. Comparative study of sliced tragal cartilage and temporalis fascia in type I tympanoplasty. J Laryngol Otol 2015;129:16-22. [Crossref] [PubMed]
- Rai AK, Singh GB, Sahu R, et al. Evaluation of simultaneous bilateral same day tympanoplasty type I in chronic suppurative otitis media. Auris Nasus Larynx 2014;41:148-52. [Crossref] [PubMed]
- Roxbury CR, Yang J, Salazar J, et al. Safety and postoperative adverse events in pediatric otologic surgery: analysis of American College of Surgeons NSQIP-P 30-Day outcomes. Otolaryngol Head Neck Surg 2015;152:790-5. [Crossref] [PubMed]
- Duval M, Grimmer JF, Meier J, et al. The effect of age on pediatric tympanoplasty outcomes: a comparison of preschool and older children. Int J Pediatr Otorhinolaryngol 2015;79:336-41. [Crossref] [PubMed]
- Knapik M, Saliba I. Pediatric myringoplasty: a study of factors affecting outcome. Int J Pediatr Otorhinolaryngol 2011;75:818-23. [Crossref] [PubMed]
Cite this article as: Chidlow C, Prunty S, Hinton-Bayre A, Shubhraj S, Renton J, Kuthubutheen J. Practice patterns in myringoplasty surgery among Australian surgeons. Aust J Otolaryngol 2020;3:28.