
Recruitment to otorhinolaryngology: opportunities abound
Introduction
Medical student interest in a surgical career is declining (1-3). Around 50% of medical students decide on their career path during their undergraduate studies (4). The clinical exposure students gain on clinical rotations is an important factor in how they perceive a specialty as a potential career option (5-7). However, medical students tend to have limited time on an otorhinolaryngology (ORL) rotation, with most being just one week long and of variable quality (8-12). This is concerning as there is a projected increase in demand for ORL surgeons in New Zealand (13). Of further concern was the finding in our recent study; just 9.4% of surveyed Year 5 medical students reported that the experience that they had received in medical school was sufficient for making informed career decisions (14).
There are a number of studies that examine factors medical students and junior doctors consider when deciding a career specialty (15-17), as well as what factors are attractive for a surgical career (6,18). There are limited data on why medical students and doctors choose ORL as a career. Of the available studies, clinical interest, work-life balance and inspiration from a senior doctor were the highest ranked factors for pursuing a career in ORL (5,19,20). However, only one study surveyed a population of ORL trainee doctors (5), and to our knowledge, none have surveyed a population of ORL surgeons.
There has been increasing interest from medical students and junior doctors to pursue specialties that are considered lifestyle-friendly, while the stereotypically career-focused surgical specialties are facing declining interest (1,15,21-23). Additionally, gender has been shown to influence career decisions, with female doctors tending to choose non-surgical careers (6,22), potentially due to gender-based bias or discrimination (6,24,25), a lack of female surgical leadership (3,6,26) and perceived compatible lifestyle choices (24,25). ORL tends to be perceived as a surgical career better for work-life balance (5,15), although there are limited studies investigating lifestyle and gender perceptions of an ORL career.
Understanding the factors that current trainees and surgeons considered important to pursuing an ORL career could help to provide guidance to medical students who are considering ORL as a career prospect.
The aims of this study were to (I) identify factors that clinicians considered important when deciding a career in ORL, (II) identify factors that medical students consider important when deciding a career and (III) compare clinician and student perspectives on the influence of mentorship, family factors and gender on career choices and ORL. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/ajo-20-34).
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the University of Auckland Human Participants Ethics Committee (Reference Number 022033) and informed consent was taken from all individual participants.
Clinicians training in ORL in New Zealand at the time of the study (“trainees”) and all those that had completed ORL training in New Zealand in the five years prior (“surgeons”) were invited to participate in the questionnaire. Fifth-year medical students (“students”) from the University of Auckland, one of two medical schools in New Zealand, who completed their 2018 academic year at Waikato Hospital, New Zealand were invited to participate (n=53). All students had completed a five-day clinical attachment in ORL at Waikato Hospital as part of the normal medical school curriculum.
Separate questionnaires were designed for clinicians (trainees and surgeons) and students using Google Forms. Participants were emailed an invitation to anonymously complete the questionnaire. Clinicians were asked questions about factors influencing their decision to pursue ORL as a career, their experiences as a medical student, mentorship, personal/social impacts of training on family and perceived gender biases in the ORL field. Students were asked about factors that may influence career choices and perceptions of mentorship, family and gender in ORL. For both clinicians and students, factors that may influence career choice were selected based off existing literature: interest in the clinical practice, interest in the pathophysiology, lifestyle (i.e., ability to pursue a family, achieve satisfactory work-life balance), opportunities for research, income, work lifestyle (i.e., workload, on-call rostering, professional environment, colleagues), prestige of career and senior role models (i.e., inspiration from a role model/mentor),
The survey used closed-response questions and a seven-point Likert scale to assess clinician/student confidence and importance placed on various factors.
The questionnaire was open for completion from October to November 2018. Responses were collected anonymously, and participation was voluntary. All questions required a response to submit the survey.
Descriptive statistics such as median (M), standard deviations (SD) and percentage proportions were calculated to summarise Likert-scale responses. To determine statistical significance between groups in Likert-scale responses, statistical analyses were conducted using JASP (version 0.10.2; JASP Team, 2019). A series of one-way ANOVAs were conducted with Group (3) as the independent variable. Assumption testing showed that all dependent variables except Student Experience did not violate the assumption of equality of variance. For Student Experience, a Welch’s ANOVA was used to correct for inhomogeneity of variances. Due to the small sample size, a Fisher’s Exact Test was conducted to assess whether the group (i.e., clinician or student) and their response to a closed question were independent. This was conducted using R. A P value <0.05 was considered statistically significant.
Results
A total of 29 clinicians (15 trainees, 14 surgeons) and 29 medical students participated in the survey (Table 1).
Table 1
| Participants | Trainees | Surgeons | Students |
|---|---|---|---|
| Eligible | 19 | 18 | 53 |
| Male | 13 | 11 | 31 |
| Female | 6 | 7 | 22 |
| Respondents (response rate %) | 15 (78.9) | 14 (77.8) | 29 (54.7) |
| Median age (years) | 35 | 37.5 | 23 |
| Male (%) | 10 (66.7) | 8 (57.1) | 16 (55.2) |
| Female (%) | 5 (33.3) | 6 (42.9) | 13 (44.8) |
ORL
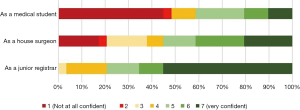
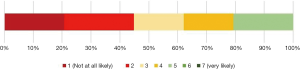
Clinicians showed increasing confidence in their choice of an ORL career as they progressed through their early career (Figure 1). Students indicated a low likelihood of pursuing ORL as a career (M=3.0, SD =1.46) (Figure 2).
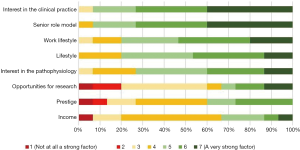
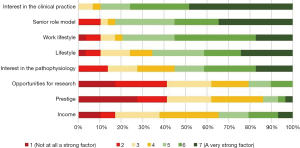
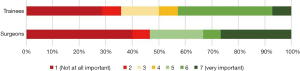
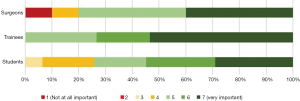
All three groups identified interest in the clinical practice, the influence of a senior role model and work lifestyle as the three strongest factors in their decision to pursue an ORL career. There were no statistically significant differences between the three groups for the three strongest factors (clinical practice: P=0.876; senior role model: P=0.426; work lifestyle: P=0.714) (Figures 3-5).

Of all clinicians, 41.4% completed an undergraduate ORL attachment of one week or shorter, as is the norm for the student group that was surveyed. Most clinicians and students believed however that a one-week ORL attachment was insufficient exposure for a student to consider ORL as a career (93.1% and 82.8% respectively).
Both surgeons (M=6.0, SD =1.33) and trainees (M=6.0, SD =1.34) thought that their experience as a medical student was moderately important to their career choice (Figure 6). Students reported that their experience in clinical attachments was important in guiding their career planning (M=5.0, SD =1.52) (Figure 7). There were no statistically significant differences between the three groups (P=0.054).

Mentorship
Most clinicians reported having a mentor at some stage in their career (75.9%). Of all clinicians, 24.1% started mentorships as students, while 10.3% of the surveyed students reported currently being in a mentorship. All three surveyed groups viewed mentorships as having high importance as part of career planning (Figure 8). There were no statistically significant differences between the three groups (P=0.199).
Family
Of all surveyed clinicians, 96.6% had a partner (surgeons: 92.9% trainees: 100%) and 58.6% had children (surgeons: 57.1%, trainees: 60%). Of the students, 65.5% had a partner and 6.9% had children. For all clinicians, 89.7% reported social or family problems due to relocation for training (surgeons: 78.6%, trainees: 100%). Of the students, 69% did not expect relocation to cause social or family problems if they were to undertake ORL training. Clinicians were 18.04 times more likely to answer “Yes” compared to students (95% CI: 4.04, 117.76; P<0.001; Fisher’s Exact Test).
Gender
Of the clinicians with mentors (n=22), 77.3% had male mentors. Four clinicians, all of whom were female, reported having a female mentor. One clinician reported having a gender diverse mentor. All students with mentors (n=3, one female, two males) reported having a male mentor.
Of the clinicians, 69% did not believe that there was a gender bias in ORL. Of the 31% that did (n=9), 77.8% believed it was in favour of males. Of the students, 69% also did not believe that there was a gender bias in ORL. All students that thought there was a gender bias (n=9) believed it was in favour of males.
Discussion
Interest in the clinical field, the influence of a senior role model and work lifestyle were the three factors rated the most important to pursuing ORL by clinicians and for future career planning by students, reproducing similar findings elsewhere (5). Despite interest in the clinical practice being considered the most important factor, the typical clinical exposure to ORL in medical school curricula is considered insufficient for career planning. The limited clinical exposure to ORL is a problem reported by other studies in the United Kingdom (8,12,27), Canada (9) and the United States (10), usually due to limited time allocated to ORL attachments in medical school curricula.
The importance of an influential senior role model and mentorship has also been highlighted in this study (Figures 3-5). However, our study demonstrates a disconnect between the perceived importance of mentorship and the number of students involved in a mentorship, particularly with female mentors. A survey of the New Zealand medical workforce found that of surveyed ORL clinicians, 20.1% were female (28). An influential role model has been shown to be a strong factor for why students consider a specialty as a future career (5,20,29-31). Mentorship also provides students with insights into clinical lifestyles and assists with personal development and career counselling (29,32).
While gender perceptions in ORL have not been extensively studied, our findings of a male-favouring bias and female-discriminating bias in surgery are not new (6,24,25). Female representation in surgery is improving but large gender gaps still exist in both absolute representation and in leadership roles (33,34). Furthermore, it is clear that women in surgery are still subject to bias and discrimination within Australasia. A 2015 survey of Royal Australasian College of Surgeons (RACS) fellows, trainees and international medical graduates found that female respondents reported higher rates of discrimination, bullying and sexual harassment (35). Unaccommodating workplace environments, challenges to credibility and lack of professional and psychological support are also just a few of the many significant issues raised by two recent qualitative studies of female RACS fellows and trainees (36,37). Both studies suggest that the under-representation and continued discrimination of females in surgery is a result of multiple systemic factors that current strategies fail to address. While increasing representation of females in surgery should be viewed positively, it is clear that there is still a need for systemic and cultural change. Failing to address the issue of gender bias in surgery will likely continue to deter female students from a surgical career, who look to their senior counterparts for insight into a surgical career (6,24).
Of all surveyed clinicians, 89.7% reported social or family difficulties due to relocation requirements during training. Strikingly however, 69% of students did not expect social or family difficulties if they were to undertake ORL training. The contrast in student perceptions or expectations of training compared to the reality is highlighted in this study but also in a recent study looking at burnout in Australian ORL trainees (38). Burnout is a prevalent issue in ORL; an American study of 182 ORL residents found that 50% of survey respondents self-reported feeling burnt out (39). While burnout is a multifactorial issue, the implementation of a mentorship system could help to support trainees navigate professional and social difficulties in settings where one’s traditional social supports may not be accessible. Mentorship could also provide students and junior doctors insight into the realities of the path that lies ahead.
A factor not included in the present study was the perception of competitiveness and ease of entering a surgical training scheme. Surgical training is stereotypically perceived as being competitive by students, which may deter application to training (23). Future studies could investigate Australasian student/junior doctor perspectives on entering a training scheme and its impact on career choice.
Our study has some limitations. The sample size is relatively small although surveying within a small community such as ours has allowed us to achieve relatively high response rates. However, the perspectives of more senior surgeons were excluded as the surgeon sub-group was limited to those who had finished ORL training in the last 5 years (n=18). This was to limit a bias of experience, where responses of more senior surgeons may be reflective of their experience as practising ORL surgeons rather than factors that they considered as students or junior doctors. Focusing on more recently qualified surgeons may also be more indicative of recent trends in ORL career choice, giving a more ‘contemporary’ perspective and allowing appropriate comparisons to current students and junior doctors. Conversely, the student subset is also very specific, using a sole cohort of students from one medical school. The inclusion of a variety of cohorts at different year levels and at a different medical school could improve generalisability of the results. Similarly, the generalisability of the study outside of New Zealand is unclear, although study results are in concordance with international literature. The investigation of Australian ORL clinician and student perspectives represents an avenue of future study.
Conclusions
There is much to be achieved with regards recruitment to a career in ORL including equity of access, mentorship of potential applicants and appropriate advice about the realities of the pressures of training. Expansion of mentorship programmes, with particular regard to potential female applicants, would be expected to be fulfilling.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/ajo-20-34
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ajo-20-34). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the University of Auckland Human Participants Ethics Committee (Reference Number 022033) and informed consent was taken from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Deedar-Ali-Khawaja R, Khan SM. Trends of surgical career selection among medical students and graduates: a global perspective. J Surg Educ 2010;67:237-48. [Crossref] [PubMed]
- von Websky MW, Oberkofler CE, Rufibach K, et al. Trainee satisfaction in surgery residency programs: modern management tools ensure trainee motivation and success. Surgery 2012;152:794-801. [Crossref] [PubMed]
- Green R, Steven R, Haddow K. Declining applications to surgical specialist training. Bull R Coll Surg Engl 2017;99:142-4. [Crossref]
- Markert RJ. Change in specialty choice during medical school. J Fam Pract 1983;17:295-300. [PubMed]
- Bhutta M, Mandavia R, Syed I, et al. A survey of how and why medical students and junior doctors choose a career in ENT surgery. J Laryngol Otol 2016;130:1054-8. [Crossref] [PubMed]
- Peel JK, Schlachta CM, Alkhamesi NA. A systematic review of the factors affecting choice of surgery as a career. Can J Surg 2018;61:58-67. [Crossref] [PubMed]
- Marshall DC, Salciccioli JD, Walton SJ, et al. Medical student experience in surgery influences their career choices: a systematic review of the literature. J Surg Educ 2015;72:438-45. [Crossref] [PubMed]
- Mace AD, Narula AA. Survey of current undergraduate otolaryngology training in the United Kingdom. J Laryngol Otol 2004;118:217-20. [Crossref] [PubMed]
- Campisi P, Asaria J, Brown D. Undergraduate otolaryngology education in Canadian medical schools. Laryngoscope 2008;118:1941-50. [Crossref] [PubMed]
- Haddad J, Shah J, Takoudes TG. A survey of US medical education in otolaryngology. Arch Otolaryngol - Head Neck Surg 2003;129:1166-9. [Crossref] [PubMed]
- Doshi J, Carrie S. A survey of undergraduate otolaryngology experience at Newcastle University Medical School. J Laryngol Otol 2006;120:770-3. [Crossref] [PubMed]
- Powell J, Cooles FAH, Carrie S, et al. Is undergraduate medical education working for ENT surgery? A survey of UK medical school graduates. J Laryngol Otol 2011;125:896-905. [Crossref] [PubMed]
- Royal Australasian College of Surgeons. Surgical workforce projection to 2025. Volume 2: The New Zealand Workforce, 2013.
- Hardcastle T, Wood A. The utility of virtual reality surgical simulation in the undergraduate otorhinolaryngology curriculum. J Laryngol Otol 2018;132:1072-6. [Crossref] [PubMed]
- Takeda Y, Morio K, Snell L, et al. Characteristic profiles among students and junior doctors with specific career preferences. BMC Med Educ 2013;13:125. [Crossref] [PubMed]
- Vo A, McLean L, McInnes MDF. Medical specialty preferences in early medical school training in Canada. Int J Med Educ 2017;8:400-7. [Crossref] [PubMed]
- Wiener-Ogilvie S, Begg D, Dixon G. Foundation doctors career choice and factors influencing career choice. Educ Prim Care 2015;26:395-403. [Crossref] [PubMed]
- Brandt MG, Scott GM, Doyle PC, et al. Otolaryngology - Head and neck surgeon unemployment in Canada: A cross-sectional survey of graduating otolaryngology - Head and neck surgery residents. J Otolaryngol Head Neck Surg 2014;43:37. [Crossref] [PubMed]
- Ranta M, Hussain SSM, Gardner Q. Factors that inform the career choice of medical students: Implications for otolaryngology. J Laryngol Otol 2002;116:839-41. [Crossref] [PubMed]
- McCaffrey JC. Medical student selection of otolaryngology-head and neck surgery as a specialty: Influences and attitudes. Otolaryngol Head Neck Surg 2005;133:825-30. [Crossref] [PubMed]
- van der Horst K, Siegrist M, et al. Residents’ reasons for specialty choice: Influence of gender, time, patient and career. Med Educ 2010;44:595-602. [Crossref] [PubMed]
- Kawamoto R, Ninomiya D, Kasai Y, et al. Gender difference in preference of specialty as a career choice among Japanese medical students. BMC Med Educ 2016;16:288. [Crossref] [PubMed]
- Hill EJ, Bowman KA, Stalmeijer RE, et al. Can I cut it? Medical students’ perceptions of surgeons and surgical careers. Am J Surg 2014;208:860-7. [Crossref] [PubMed]
- Hill E, Vaughan S. The only girl in the room: How paradigmatic trajectories deter female students from surgical careers. Med Educ 2013;47:547-56. [Crossref] [PubMed]
- Fitzgerald JE, Tang SW, Ravindra P, et al. Gender-related perceptions of careers in surgery among new medical graduates: results of a cross-sectional study. Am J Surg 2013;206:112-9. [Crossref] [PubMed]
- Weiss A, Lee KC, Tapia V, et al. Equity in surgical leadership for women: more work to do. Am J Surg 2014;208:494-8. [Crossref] [PubMed]
- Easto RH, Reddy V. A survey of ENT experience in South West Peninsula general practitioner trainees: How can post-graduate ENT training be improved? J Laryngol Otol 2016;130:893-6. [Crossref] [PubMed]
- Medical Council of New Zealand. The New Zealand Medical Workforce in 2017 [Internet] 2017. Available online: https://www.mcnz.org.nz/assets/Publications/Workforce-Survey/c3f49fa2d2/Workforce-Survey-Report-2017.pdf
- Frei E, Stamm M, Buddeberg-Fischer B. Mentoring programs for medical students - A review of the PubMed literature 2000-2008. BMC Med Educ 2010;10:32. [Crossref] [PubMed]
- Ravindra P, Fitzgerald JEF. Defining surgical role models and their influence on career choice. World J Surg 2011;35:704-9. [Crossref] [PubMed]
- Quillin RC 3rd, Pritts TA, Davis BR, et al. Surgeons underestimate their influence on medical students entering surgery. J Surg Res 2012;177:201-6. [Crossref] [PubMed]
- Gurgel RK, Schiff BA, Flint JH, et al. Mentoring in otolaryngology training programs. Otolaryngol Head Neck Surg 2010;142:487-92. [Crossref] [PubMed]
- Abelson JS, Chartrand G, Moo TA, et al. The climb to break the glass ceiling in surgery: Trends in women progressing from medical school to surgical training and academic leadership from 1994 to 2015. Am J Surg 2016;212:566-572.e1. [Crossref] [PubMed]
- Epperson M, Gouveia CJ, Tabangin ME, et al. Female representation in otolaryngology leadership role. Laryngoscope 2020;130:1664-9. [Crossref] [PubMed]
- Crebbin W, Campbell G, Hillis DA, et al. Prevalence of bullying, discrimination and sexual harassment in surgery in Australasia. ANZ J Surg 2015;85:905-9. [Crossref] [PubMed]
- Hutchison K. Four types of gender bias affecting women surgeons and their cumulative impact. J Med Ethics 2020;46:236-41. [Crossref] [PubMed]
- Liang R, Dornan T, Nestel D. Why do women leave surgical training? A qualitative and feminist study. Lancet 2019;393:541-9. [Crossref] [PubMed]
- Raftopulos M, Wong EH, Stewart TE, et al. Occupational burnout among otolaryngology-head and neck surgery trainees in Australia. Otolaryngol Head Neck Surg 2019;160:472-9. [Crossref] [PubMed]
- Reed L, Mamidala M, Stocks R, et al. Factors correlating to burnout among Otolaryngology residents. Ann Otol Rhinol Laryngol 2020;129:599-604. [Crossref] [PubMed]
Cite this article as: Yeom BW, Hardcastle T, Wood AJ. Recruitment to otorhinolaryngology: opportunities abound. Aust J Otolaryngol 2020;3:27.


