Intraoperative acupuncture as complementary analgesic for post-tonsillectomy pain in children—a prospective randomised clinical trial of effects and safety
Introduction
Tonsillectomy is one of the most commonly performed surgical procedures in children and often accompanied by significant postoperative morbidity, including bleeding, pain, nausea, vomiting, poor oral intake and dehydration.
Most strategies for managing postoperative pain after tonsillectomy utilise oral drug combinations such as paracetamol or acetaminophen, non-steroid anti-inflammatory drugs (NSAIDS), gabapentin and opioids (1-4). However, post-tonsillectomy pain can lead to poor oral intake and hence limit the effectiveness of such treatment.
As a non-drug treatment, acupuncture may be useful in complementing the analgesic effect of these postoperative drugs and reducing their side effects (5-8).
We designed a randomised, controlled trial to examine the effect of intraoperative acupuncture on postoperative pain in children undergoing adenotonsillectomy. We present this article in accordance with the CONSORT guidelines (available at http://dx.doi.org/10.21037/ajo-19-74).
Methods
The study was conducted in accordance with the National Statement on Ethical Conduct in Human Research [2015] and was approved by the Greenslopes Research and Ethics Committee and the St Vincent’s Health and Aged Care Human Research Ethics Committee. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
We enrolled 251 children undergoing elective adenotonsillectomy into our study.
All children were aged between 2 to 10 years old and otherwise healthy with ASA 1 or 2 status.
Exclusion criteria included any significant allergy, known bleeding tendency, known or likely airway difficulty and children who had received acupuncture, analgesics or sedatives within 36 hours prior to surgery.
All suitable patients (253 in total) were invited to participate in the study and all but 2 of the parents accepted and consented. One parent felt that the whole hospital experience was too stressful and did not want any additional stress. The other parent did not give a reason for the refusal.
All parents gave written informed consent prior to surgery. All parents were interviewed and consented by the anaesthetist the night before or on the day of surgery. All were given a chance to ask questions at the interview and any queries were addressed prior to the procedure.
The patients were randomised in blocks of 50 and assigned by a computer-generated programme to either a control or acupuncture group. To minimise allocation bias, this procedure was undertaken by an independent collaborator. On the day of surgery, the independent collaborator would receive the names of the patients and then allocate the patients into the respective groups. The anaesthetist was informed just prior to the procedure of their allocations. The patients and all subsequent persons recording the pain assessments including parents, recovery nurses, ward nurses and follow-up research nurses were blinded as to which group each patient was assigned.
In the operating room, the same designated drugs, in particular Morphine, Granisetron, Dexamethasone, Clonidine and Paracetamol were drawn up in the correct weigh adjusted dosage by the anaesthetist prior to starting the procedure and crossed-checked by an independent anaesthetic nurse assigned to the list for that day to minimise bias in drug administration.
In the control group, each child was accompanied by their parent into the operating room for induction. General anaesthesia was induced by 40% oxygen, 60% nitrous oxide and 8% Sevoflurane until loss of consciousness. The parent was then escorted out of the operating room. An intravenous cannula was inserted and the child was given morphine 0.1 mg/kg, granisetron 20 mcg/kg, dexamethasone 0.1 mg/kg, clonidine 1 mcg/kg and paracetamol 15 mg/kg intravenously. A flexible laryngeal mask (LMA) of the appropriate size was inserted to maintain the airway for the duration of surgery and recovery. Anaesthesia was maintained with oxygen 100% and end-tidal sevoflurane of 4–6% with spontaneous ventilation. An intravenous fluid bolus of 10 mL/kg was given intraoperatively and followed by 1 mL/kg/h in the ward. The adeno-tonsillectomy procedure was performed by blunt dissection and electrocautery. At the conclusion of surgery, the child was transferred onto a ward bed and taken to recovery with the LMA in situ. The LMA was removed in recovery when the child was awake and able to maintain his/her own airway.
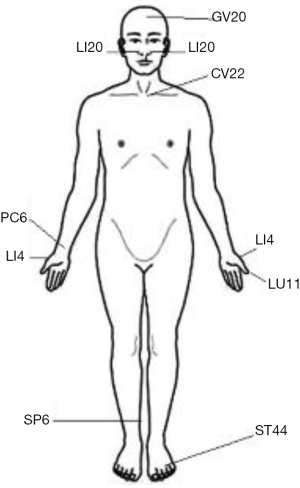
In the acupuncture group, an identical procedure to that described above was followed with the addition of the insertion of ten (9) acupuncture needles after LMA insertion and prior to surgical stimulation. All acupuncture was performed by a single anaesthetist who had prior certification from the Australian Medical Acupucnture College (AMAC). Stainless steel acupuncture needles, 15 mm in length and 0.18 mm in diameter (Serin Co, Shizuoka, Japan), were used. The sites of needle insertion, in accordance Chinese Medicine standards, were: LI4 bilaterally, LI20/Bitong bilaterally, CV(REN)22, GV(DU)20, LU11, PC6, ST44, SP6 (Figure 1). These particular acupuncture points were selected for their local analgesic properties in the nasopharyngeal region or for their general analgesic and anti-inflammatory properties. No electrical stimulation or manual stimulation was applied to the acupuncture needles. Surgery was commenced immediately following the acupuncture needle insertion. The needles were left in situ for the duration of surgery, and immediately removed at the completion of surgery prior to the transfer of patient to recovery room.
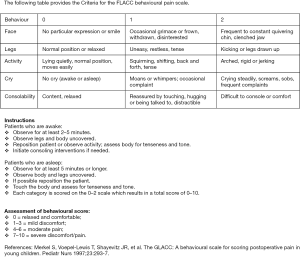
In recovery and on the ward, all patients were assessed for pain using the Face, Legs, Activity, Cry, Consolability (FLACC) pain scale (Figure S1) by nursing staff. The FLACC Pain Scale is a widely used behavioural observation pain scales to quantify procedural pain in infants and young children (10) and has been shown to be particularly useful in assessing postoperative tonsillectomy pain in paediatric patients (9).
In recovery, at intervals of 10, 20, 30, and 45 minutes after awakening, if the child showed evidence of significant pain with a pain score of ≥7 on the FLACC scale which was unrelieved by simple comfort measures including nursing by parents or taking oral ice blocks, he/she was treated with a Morphine bolus of 50 mcg/kg. The patient was also assessed for nausea and vomiting and treated with Droperidol 10 mcg/kg if required. When the child was awake, alert and comfortable, he/she was discharged to the ward with the accompanying parent and ward nurse.
On the ward, all patients were given regular Paracetamol 15 mg/kg orally every 6 hours. If the child showed evidence of significant pain with a pain score of ≥7 on the FLACC scale, oxycodone liquid 0.1 mg/kg was given at 4 hourly intervals as required at the discretion of the ward nurse. All patients were encouraged to eat and drink as tolerated. All observations, including pain score and pulse oximetry, were recorded by the ward nurse at 1 to 2 hourly intervals, together with the time and dose of oxycodone administered postoperatively. All patients were given another dose of Dexamethasone 10 mcg/kg orally on the first postoperative morning. They were then discharged if they were able to eat and drink. If the patient was still in significant pain, or not tolerating oral intake, then he/she would remain in hospital until these issues were overcome.
All patients were followed up by telephone interview on days 1, 3 and 5 after discharge from hospital by a blinded, independent research nurse. A pain assessment was made at home for each morning, afternoon and evening by the parents using the same FLACC scale.
For concealment, all patient details were entered into a cloud-based database by the blinded collaborator and the results subsequently were entered by the blinded research nurses.
The primary objective of this study was to assess if intraoperative acupuncture can reduce the postoperative pain score for children following adenotonsillectomy as measured by the FLACC pain scale.
A secondary objective of the study was to assess if intraoperative acupuncture can also reduce the oxycodone requirement for children following adenotonsillectomy.
Power analysis
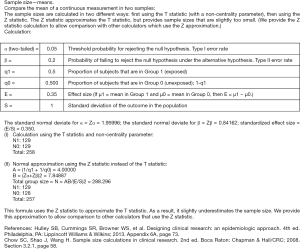
During our ascertainment period in the first nine months of 2015, we observed that by using supplemental acupuncture intraoperatively, there appeared to be approximately a one-third reduction in the dose of intraoperative Morphine required to achieve similar patient comfort level in recovery. Subsequent assessment of our preliminary study data suggested a 30% to 35% postoperative reduction in the Pain Scores with the addition of intraoperative acupuncture. Based on these observations, we estimate that between 100 to 150 patients are required in each group to achieve a level of statistical significance (P<0.05) at a power of 90% (Figure S2). We also noted that an earlier study with a similar design to ours used an initial 35% difference to arrive at a sample size of 30 for each group but was subsequently found to be underpowered (11). A subsequent editorial examined the results of that study and their power recalculation was made post-hoc, revealing an estimate sample size of 260 patients was required for statistical significance (12). Our own power analysis resulted similarly in a sample size of 258 patients, which was comparable to the number of patients [251] enlisted in our study during the 18 months period.
Statistical analysis
All statistical analysis was performed by an independent statistician. Differences in demographic data were analysed using t-tests for continuous variables and chi-squared tests for categorical variables. Outcome data were analysed using simple linear regression for continuous variables and logistic regression for categorical variables. Data analysis was conducted using Stata v14.2 (StataCorp, College Station, TX, USA).
Results
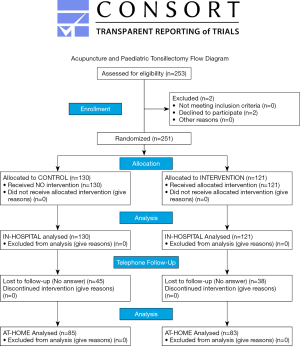
We recruited 251 patients between June 2016 and September 2018 in the study, and all completed the protocol for measurements of the primary and secondary objectives. Of the 251 children enrolled, 121 (48%) received acupuncture in the treatment group and 130 (52%) were in the control group.
Figure 2 shows the CONSORT diagram, and Table 1 shows the distribution and characteristics of patients. There was no demographic difference between the acupuncture and the control groups.
Table 1
| Characteristics | Control (n=130) | Acupuncture (n=121) |
|---|---|---|
| Age, years | 4.6 (2.1) | 4.9 (2.1) |
| Weight, kg | 21.6 (8.9) | 21.0 (8.4) |
| Sex, male | 82 | 80 |
| Duration of surgery, min | 24.8 (7.7) | 25.2 (7.1) |
Values are shown as mean (SD) or number (proportion).
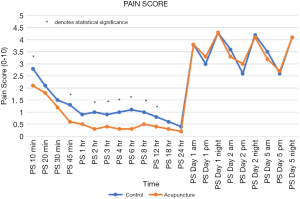
Differences in Pain Scores between the two groups are shown in Table 2 and Figure 3.
Table 2
| Pain score period | Control | Acupuncture | Simple linear regression | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean | SD | N | Mean | SD | Coefficient | P value | |||
| PS 10 min | 130 | 2.8 | 3.2 | 121 | 2.1 | 2.7 | −0.7 | 0.052 | ||
| PS 20 min | 130 | 2.1 | 2.6 | 121 | 1.8 | 2.4 | −0.3 | 0.336 | ||
| PS 30 min | 115 | 1.5 | 2.4 | 105 | 1.2 | 1.8 | −0.4 | 0.205 | ||
| PS 45 min | 69 | 1.3 | 2.4 | 63 | 0.6 | 1.2 | −0.7 | 0.036 | ||
| PS 1 h | 130 | 0.9 | 1.8 | 120 | 0.5 | 1.2 | −0.4 | 0.058 | ||
| PS 2 h | 129 | 1 | 1.8 | 119 | 0.3 | 0.8 | −0.7 | 0 | ||
| PS 3 h | 129 | 0.9 | 1.7 | 117 | 0.4 | 0.9 | −0.5 | 0.005 | ||
| PS 4 h | 129 | 1 | 1.8 | 118 | 0.3 | 0.8 | −0.7 | 0 | ||
| PS 6 h | 128 | 1.1 | 1.9 | 117 | 0.3 | 0.9 | −0.8 | 0 | ||
| PS 8 h | 127 | 1 | 1.8 | 116 | 0.5 | 1.1 | −0.4 | 0.027 | ||
| PS 12 h | 124 | 0.8 | 1.6 | 115 | 0.4 | 1 | −0.4 | 0.044 | ||
| PS 18 h | 111 | 0.6 | 1.5 | 108 | 0.3 | 0.9 | −0.3 | 0.096 | ||
| PS 24 h | 50 | 0.4 | 1 | 61 | 0.2 | 0.7 | −0.1 | 0.472 | ||
| PS Day 1 am | 83 | 3.8 | 2.7 | 84 | 3.8 | 2.6 | 0.1 | 0.902 | ||
| PS Day 1 pm | 83 | 3 | 2.5 | 85 | 3.3 | 2.4 | 0.3 | 0.368 | ||
| PS Day 1 night | 82 | 4.3 | 2.6 | 85 | 4.3 | 2.7 | 0 | 0.908 | ||
| PS Day 2 am | 83 | 3.6 | 2.4 | 85 | 3.3 | 2.4 | −0.3 | 0.373 | ||
| PS Day 2 pm | 83 | 2.6 | 2.6 | 85 | 3 | 2.5 | 0.5 | 0.23 | ||
| PS Day 2 night | 83 | 4.2 | 2.6 | 85 | 4.1 | 2.7 | −0.1 | 0.786 | ||
| PS Day 5 am | 81 | 3.5 | 2.5 | 84 | 3.2 | 2.5 | −0.3 | 0.475 | ||
| PS Day 5 pm | 81 | 2.6 | 2.6 | 84 | 2.7 | 2.6 | 0.2 | 0.676 | ||
| PS Day 5 night | 80 | 4.1 | 2.6 | 79 | 4.1 | 2.8 | 0 | 0.974 | ||
Patients who received acupuncture experienced significantly less pain than the patients in the control group during their stay in hospital (Table 2 and Figure 3). In the Recovery Room, although the Pain Score at 10 minutes postoperatively did not show significant difference at P=0.52, the Pain Score at 45 minutes showed strong evidence of difference at P=0.036. On the ward, the differences in Pain Scores between the acupuncture and control groups were even more noticeable. There was strong evidence of differences in Pain Scores between the two groups from 2 to 12 hours postoperatively, with all recordings within this period showing a statistically significant reduction in pain in the acupuncture group (P=0.001–0.044).
In the latter portion of the patients’ hospital stay between 18 and 24 hours post-operatively, the evidence of differences in the groups’ Pain Scores were much weaker, trending away from statistical significance, with P=0.096 at 18 hours and P=0.472 at 24 hours. It should be noted that less data were recorded at his later time because either it was night time and these children were not disturbed from sleep or because the children undergoing an afternoon procedure were not present for this period if they were routinely discharged the following morning.
While a number of patients reported high Pains Scores at times, a large proportion of patients reported their Pain Score as zero, causing the data distribution to skew towards zero. This accounts for the lower mean Pain Score than expected at all time points. As expected with paediatric pain assessments, there is a very high degree of variability, as exemplified by the large standard deviation. However, given our large sample size, we were able to perform a linear regression which demonstrated significant differences between the groups. This means that while the differences in Means between control and acupuncture groups may be small, they reflect much bigger differences in actual Pain Scores between patients due to the skewed distribution and high variability.
There were no statistically significant differences in Pain Scores following discharge between the treatment and control groups at home.
However, there were a number of parents who did not return the follow-up telephone calls and as such, our data set is much smaller, with only 168 respondents out of a total of 251 (67%) represented, including 85 patients in control group (34%) and 83 patients in acupuncture group (31%).
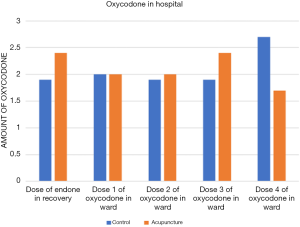
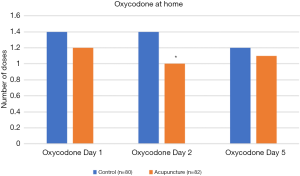
There was no statistical difference in the dose of Oxycodone administered in hospital between the two groups (Table 3 and Figure 4). However, an overall trend of lower Oxycodone requirement was noted in the acupuncture group at home over all three days recorded, reaching statistical significance (P=0.035) on postoperative day 2 (Table 4 and Figure 5).
Table 3
| Oxycodone in hospital | Control | Acupuncture | Simple linear regression | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean | SD | N | Mean | SD | Coefficient | P value | |||
| Dose of Endone in recovery | 8 | 1.9 | 0.6 | 5 | 2.4 | 0.5 | 0.5 | 0.174 | ||
| Dose 1 of oxycodone in ward | 105 | 2 | 0.9 | 96 | 2 | 0.8 | 0 | 0.954 | ||
| Dose 2 of oxycodone in ward | 70 | 1.9 | 0.8 | 65 | 2 | 0.8 | 0.1 | 0.519 | ||
| Dose 3 of oxycodone in ward | 32 | 1.9 | 0.9 | 28 | 2.4 | 2.1 | 0.6 | 0.185 | ||
| Dose 4 of oxycodone in ward | 10 | 2.7 | 3.5 | 6 | 1.7 | 0.5 | −1 | 0.489 | ||
Table 4
| Oxycodone at home | Control | Acupuncture | Simple linear regression | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean | SD | N | Mean | SD | Coefficient | P value | |||
| Day 1 | 80 | 1.4 | 1.2 | 82 | 1.2 | 1.1 | −0.2 | 0.253 | ||
| Day 2 | 80 | 1.4 | 1.3 | 80 | 1 | 1.1 | −0.4 | 0.035 | ||
| Day 5 | 78 | 1.2 | 1.3 | 76 | 1.1 | 1.3 | −0.2 | 0.36 | ||
There were no clinically significant complications resulting from the acupuncture treatment, with no local neurological or systemic complication reported by the staff or the parents. The only notable complication was minor bleeding at the sites of needle insertion following their withdrawals, occurring in 3 patients (2.5%), most commonly around the alar area (LI20) and the thumb nail (LU11). This was treated with locally applied pressure and in all cases, stopped within 10 seconds, before the patients were transferred to recovery. Unlike most other studies (13,14), erythema around the needle insertion sites was uncommon, being noted in only 2 patients (1.7%), around the thenar eminence (LI4). No haematoma was noted or reported in any patients.
Overall, 16 patients were readmitted for postoperative bleeding (6.4%), with 8 patients each from control and acupuncture group. Of these, 6 patients (2.4%) returned to operating theatre for control of bleeding, comprising of 3 patients each from control and acupuncture groups. In addition, 4 patients were re-admitted following discharge. Two patients had poor pain control and were not tolerating oral medications, both from the control group. Two patients were admitted for a likely viral upper respiratory tract infection, both from the acupuncture group.
Discussion
In Australia, pain relief following adenotonsillectomy in children commonly consists of Paracetamol, Non-steroidal anti-inflammatory drugs (NSAIDs), and narcotics such as oral Oxycodone or Codeine. Although such treatment is generally highly effective, the use of opioid medications can precipitate or exacerbate nausea, vomiting, respiratory suppression or occasionally, as seen in some well-publicized cases, result in fatalities (15).
Our results show that acupuncture is an effective supplemental adjunct for optimizing postoperative pain relief in children undergoing adenotonsillectomy. While our current drug regimen is largely satisfactory, with most children reporting adequate pain control during their stay in hospital, it was enhanced by the addition of intraoperative acupuncture treatment. This was particularly noticeable in the period between 2 and 12 hours postoperatively, during which there were statistically significant differences in pain scores between the acupuncture and control groups. This is a particularly important period for these children because they are normally awake, active, eating and drinking during this time.
In contrast to the significantly lowered pain score in the acupuncture group, there was no significant differences between the two groups in terms of the number of doses or the amount of oxycodone given in hospital. While there was an overall lower trend for fewer doses given in the acupuncture group in comparison to the control group, it did not reach statistical significance. This was both surprising and disappointing, as we would have expected a lower pain score to result in a reduced requirement for a rescue medication such as oxycodone. These results might reflect a flaw in our methodology, in that we did not communicate and educate our ward nurses sufficiently about our study. It is probable that the nurses on the ward have routinely given the children oxycodone for postoperative pain prior to the study and continued to do so during the study, even if the pain score was reduced. In particular, some nurses routinely gave children oxycodone before bedtime to reduce the possibility of them waking up in pain at night, instead of using it as needed, and thus potentially obscuring any possible benefit from acupuncture at this time. This would fit in with the measured mean time to first dose of oxycodone of between 8 and 10 hours, which was slightly longer in the acupuncture group (9.44±4.75) than the control (8.39±5.0) but did not reach statistically significance (P=0.13).
In our follow-up at home, there was no demonstrable difference in pain scores between the two groups during the first 5 days following discharge from hospital. However, there is an overall lower oxycodone requirement in the acupuncture group at home in all three measuring days. In particular, there was a significant decrease in the number of oxycodone doses required in the acupuncture group on day 2. This could possibly be due to the well-being effects of acupuncture (16). It may be that the acupuncture children recovered better, being more active and feeling better than the control children in the postoperative period at home, resulting in less need for oxycodone.
We cannot readily account for the discrepancies between the pain score and the oxycodone requirement at home. One explanation could be that these pain scores at home were recorded by parents and not by nurses, resulting in greater variability. Parents only measured pain score 3 times a day at home which is much less frequent than the 1 to 2 hour interval measurements in hospital, resulting in less accuracy. It may also be that the timing of the oxycodone doses coincided with the time of pain score measurements, thus partly obscuring any noticeable differences between the two groups. In any case, a reduced postoperative requirement for oxycodone would be a strong argument in favour of the use of intraoperative acupuncture in children undergoing adenotonsillectomy.
To extend the benefits of acupuncture further into the postoperative period, we could have utilised a number of additional techniques, such as intraoperative electroacupuncture, repeated acupuncture on the ward and/or attaching indwelling acupuncture micro-pins prior to home discharge. However, we considered these techniques to be more invasive and hence less likely to be accepted by parents and children. In our similar concurrent study of acupuncture for post-tonsillectomy pain in adults, in addition to intraoperative acupuncture, we inserted indwelling micro-pins on patients’ earlobes, as part of a well-described auricular acupuncture technique, to assess the benefits of ongoing acupuncture treatment at home. This seemed to be very well tolerated by our adult patients and may be applicable in children in future.
Recent evidences in literature indicate that acupuncture may have a role in reducing postoperative pain and vomiting for tonsillectomy in children (5-8). This would then reduce their opioid requirement and, in turn, reduce undesirable drug side effects.
In a study of 143 adult patients, Sertel et al. showed that acupuncture significantly reduced odynophagia following tonsillectomy; however, this study employed only post-procedure inpatient acupuncture combined with NSAIDs administration (5). It suggests that acupuncture may be as effective as NSAIDs for treating odynophagia following tonsillectomy.
In a similarly designed study of 60 children, Gilbey et al. showed that, in the treatment group, there was less pain, reduced oral analgesic requirement, and higher patient/parent satisfaction with analgesic treatment scores (7). No adverse effects were recorded. They concluded that acupuncture, in addition to conventional analgesic treatment, is an effective treatment for post-tonsillectomy pain. They also noted that acupuncture is safe and well received by children and their parents.
Both these studies suggest that acupuncture may have a significant role in reducing postoperative tonsillectomy pain. However, performance of acupuncture in children who are awake is unlikely to gain wide acceptance.
In a study of intraoperative acupuncture and post-tonsillectomy pain in 59 children, Tsao et al. found there were no significant differences in opioid dose administered in hospital or total postoperative length of stay between the control and treatment groups (6). However, the clinical trends were suggestive of improvements in the treatment group and the authors suggested the study was insufficiently powered to detect a statistical difference. Assessments following discharge, however, revealed significant improvements in postoperative pain control (P=0.0065) and earlier oral intake (P=0.01) in the acupuncture treatment group. By contrast, our larger sample study demonstrated reduced pain score in hospital, but not following discharge, in the treatment group.
Similarly, in a retrospective study of 57 children with postoperative tonsillectomy pain, Occhi found that intraoperative acupuncture significantly decreased pain for up to 72 hours after treatment (8). In separate study of 60 children, Lin et al. found that intraoperative acupuncture reduced pain and agitation after myringotomy (17). These studies suggest that intraoperative acupuncture may have significant benefits for up to 72 hours following treatment.
Finally, in a recent meta-analysis of 12 studies and 1,025 patients, Cho et al. noted that the pain score reported by patients in the first 48 postoperative hours as well as the postoperative analgesic requirements were significantly lower in the acupuncture group compared with the control group (18). No major adverse effects of perioperative acupuncture were reported in the enrolled studies. They concluded that perioperative acupuncture may provide pain relief without side effects in patients undergoing tonsillectomy. However, there were high levels of heterogeneity in several of the measured parameters, and the authors suggested that additional well-designed trials are required to further support the results of their meta-analysis.
The National Institutes of Health Consensus Statement asserts that one of the advantages of acupuncture is its substantially lower incidence of adverse effects in comparison with many drugs or other accepted procedures used to treat the same conditions (19). In this paper, the adverse effects related to acupuncture were reported in four studies. However, because the reported outcomes were different among the various studies, meta-analysis was not possible. Adverse effects included micro-hematoma, erythema or numbness at the acupuncture site, light-headedness, needle pain and discomfort caused by acupressure bandage. All these minor effects resolved quickly and spontaneously, thus demonstrating that adverse effects of acupuncture are minimal. Similarly, in our study, the only notable side-effects were minor bleeding that either resolved spontaneously or after a few seconds with digital pressure.
We believe that it is feasible to adopt intraoperative acupuncture into routine ENT surgical practice. Our study was indeed inspired by the works of Dr. James Ochi, an ENT Specialist in San Diego, who incorporated similar acupuncture techniques into his routine adenotonsillectomy surgical procedure, after achieving his American Board certification in Medical Acupuncture and persuading his anaesthetic colleagues to do the same. While achieving accreditation and competency for acupuncture involves many years of study and practice, this particular set of acupuncture procedure for tonsillectomy is relatively straight forwards and we believe it does not require the doctors involved to master all the nuances of acupuncture to perform this safely. One particular advantage is that anaesthetists and surgeons are already familiar with the anatomy involved for needle placements and are more than capable of treating the possible uncommon complications thereof, including dizziness, nausea or bleeding. Most parents in our study appeared to be highly receptive to their children undergoing intraoperative acupuncture with only 2 out of 253 (<1%) declining to participate. The total cost of 10 Seirin acupuncture needles is about $2.00 AUD, with a box of 100 needles costing $19.95 plus delivery—a comparatively modest amount relative to the total cost of the procedure. We did not carry out a full cost-benefit analysis but, as this single treatment of intraoperative acupuncture can improve postoperative pain relief for at least 12 hours and also reduce the oxycodone requirement at home, we believe it is a highly cost-effective intervention.
Conclusions
In conclusion, the results of our study support the current literature in finding that acupuncture is an effective supplemental tool for reducing early postoperative pain and Oxycodone requirement after discharge in children following adenotonsillectomy.
Acknowledgments
The authors thank the nursing staff at the Northwest Private Hospital and the St Vincent’s Northside Private Hospital, particularly Mrs Helen Rose and Mrs Erin Groom, for their assistance.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CONSORT reporting checklist. Available at http://dx.doi.org/10.21037/ajo-19-74
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ajo-19-74). HB serves as an unpaid editorial board member of Australian Journal of Otolaryngology from Jan 2019 to Dec 2020. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study is in accordance with the National Statement on Ethical Conduct in Human Research (2015) and was approved by the Greenslopes Research and Ethics Committee and the St Vincent’s Health and Aged Care Human Research Ethics Committee (ACTRN12619000922178) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hanasono MM, Lalakea ML, Mikulec AA, et al. Perioperative steroids in tonsillectomy using electrocautery and sharp dissection techniques. Arch Otolaryngol Head Neck Surg 2004;130:917-21. [Crossref] [PubMed]
- Moir MS, Bair E, Shinnick P, et al. Acetaminophen versus acetaminophen with codeine after pediatric tonsillectomy. Laryngoscope 2000;110:1824-7. [Crossref] [PubMed]
- St Charles CS, Matt BH, Hamilton MM, et al. A comparison of ibuprofen versus acetaminophen with codeine in the young tonsillectomy patient. Otolaryngol Head Neck Surg 1997;117:76-82. [Crossref] [PubMed]
- Sutters KA, Miaskowski C, Holdridge-Zeuner D, et al. A randomized clinical trial of the effectiveness of a scheduled oral analgesic dosing regimen for the management of postoperative pain in children following tonsillectomy. Pain 2004;110:49-55. [Crossref] [PubMed]
- Sertel S, Herrmann S, Greten HJ, et al. Additional use of acupuncture to NSAID effectively reduces post-tonsillectomy pain. Eur Arch Otorhinolaryngol 2009;266:919-25. [Crossref] [PubMed]
- Tsao GJ, Messner AH, Seybold J, et al. Intraoperative acupuncture for post-tonsillectomy pain: a randomized, double-blind, placebo-controlled trial. Laryngoscope 2015;125:1972-8. [Crossref] [PubMed]
- Gilbey P, Bretler S, Avraham Y, et al. Acupuncture for posttonsillectomy pain in children: a randomized, controlled study. Paediatr Anaesth 2015;25:603-9. [Crossref] [PubMed]
- Ochi JW. Acupuncture instead of codeine for tonsillectomy pain in children. Int J Pediatr Otorhinolaryngol 2013;77:2058-62. [Crossref] [PubMed]
- Redmann AJ, Wang Y, Furstein J, et al. The use of the FLACC pain scale in pediatric patients undergoing adenotonsillectomy. Int J Pediatr Otorhinolaryngol 2017;92:115-8. [Crossref] [PubMed]
- Crellin DJ, Harrison D, Santamaria N, et al. The Psychometric Properties of the FLACC Scale Used to Assess Procedural Pain. J Pain 2018;19:862-72. [Crossref] [PubMed]
- Dingemann J, Plewig B, Baumann I, et al. Acupuncture in post-tonsillectomy pain: A prospective, double-blinded, randomized, controlled trial. HNO 2017;65:73-9. [Crossref] [PubMed]
- Shin BC. Acupuncture for post-tonsillectomy pain: evidence from a recent randomized clinical trial. Longhua Chin Med 2018;1:11. [Crossref]
- White A. A cumulative review of the range and incidence of significant adverse events associated with acupuncture. Acupunct Med 2004;22:122-33. [Crossref] [PubMed]
- Jindal V, Ge A, Mansky P. Safety and efficacy of acupuncture in children: A review of the evidence. J Pediatr Hematol Oncol 2008;30:431-42. [Crossref] [PubMed]
- Ciszkowski C, Madadi P, Phillips MS, et al. Codeine, ultrarapid-metabolism genotype, and postoperative death. N Engl J Med 2009;361:827-28. [Crossref] [PubMed]
- White A, Cummings M, Filshie J. An introduction to Western Medical Acupuncture. London: Churchill Livingstone Elsevier, 2008: 54.
- Lin YC, Tassone RF, Jahng S, et al. Acupuncture management of pain and emergence agitation in children after bilateral myringotomy and tympanostomy tube insertion. Paediatr Anaesth 2009;19:1096-101. [Crossref] [PubMed]
- Cho HK, Park IJ, Jeong YM, et al. Can perioperative acupuncture reduce the pain and vomiting experienced after tonsillectomy? A meta-analysis. Laryngoscope 2016;126:608-15. [Crossref] [PubMed]
- NIH Consensus Conference. Acupuncture. JAMA 1998;280:1518-24. [PubMed]
Cite this article as: Ho D, Cooke K, Burns H, McCrystal D, Canty P, Barr R. Intraoperative acupuncture as complementary analgesic for post-tonsillectomy pain in children—a prospective randomised clinical trial of effects and safety. Aust J Otolaryngol 2020;3:26.