
A randomised control trial to evaluate a novel 3D animation for patient education on Menière’s disease
Introduction
Menière’s disease (MD) is a progressive and debilitating disease of the inner ear, impacting hearing and balance (1). Symptoms include tinnitus, vertigo, aural fullness and hearing loss (2-4). MD attacks tend to occur episodically with periods of normal inter-episodic functioning. There is however, a cumulative effect due to the damage caused during a MD attack with a significant reduction in quality of life.
The challenge with MD education is that it is dependent on a basic understanding of the 3D anatomy and physiology of the ear. Only with this knowledge, can a patient understand the context of what is happening to their body during these disabling attacks and the proposed goals of treatment, in the context that the true aetiology of MD is still poorly understood.
Traditional education techniques involve diagrammatic representation of anatomy and physiology of the ear with someone explaining these concepts. For some patients, a two-dimensional or heavily annotated image can be challenging to visualise and comprehend what is occurring within their body (5).
With this consideration, there is evidence that many patients with MD feel that they do not receive sufficient information from their medical practitioner, and do not feel supported by them (6,7). As a result, patients seek additional information from websites, which may be confusing, conflicting or inaccurate (6), yet effective education has been shown to be one of the most effective ways of reducing psychological stressors (1).
Whilst there is a growing body of literature demonstrating the usefulness of multimedia-based tools for patient education, there is no existing data on the use of these tools in relation to MD. Given the complex anatomy and physiology of the inner ear, the lack of knowledge of the aetiology of the disease, its disabling nature and also the significant lifestyle change of treatment and its impact on the family, there is need for better clinically driven education methods, such as multimedia-based tools.
We present the following article in accordance with the CONSORT reporting checklist (available http://dx.doi.org/10.21037/ajo-19-71).
Methods
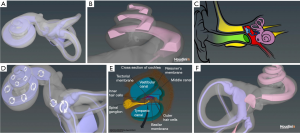
The primary study objective was to assess participant understanding of MD when using traditional education tools in comparison to the addition of a digital 3D animation (Figure 1) with the same tools.
Human research and ethics committee approval was obtained from Adventist HealthCare Limited Human Research Ethics Committee (2017-044). This study was conducted at a single-site at the Sydney Adventist Hospital in the senior author’s ENT clinic. The authors confirm that written informed consent was obtained from the patient for publication of this article and any accompanying images.
Sample selection
Inclusion criteria was any individual over the age of 18, without prior knowledge of MD. MD patients were excluded due to several confounding variables that may affect the outcome such as hearing loss, unwellness from vertigo, tinnitus, anxiety and most importantly prior knowledge. Most patients who present to an Otologist after referral from a physician or emergency department with symptoms of MD, have often been given some information about MD (which may or may not be accurate) or have already accessed information on the internet and this prior knowledge would be difficult to standardise despite randomisation. Therefore, only healthy subjects were used in this study.
Instead, to explore disease specific challenges that the animation was anticipated to address, 10 specialist otolaryngologists with experience in seeing Menière’s patients were recruited.
They were shown the video and given a five-question survey with quantitative and qualitative feedback exploring challenges in communicating with MD patients and the value of the animation in clinical practice.
Randomisation of the participants was performed using sealed envelopes containing group allocations (either 3D animation or control) which were allocated as subjects were interviewed. There was equal probability (1:1 allocation ratio) of assignment to the 3D (test) or traditional education (control) group and each session was allocated 10 minutes.
Both groups received the same verbal information assisted with an illustrated colour diagram of the ear provided by ASOHNS (Australian Society of Otolaryngology and Head and Neck Surgery). The test group had the same aforementioned education as well as a 3D animation (approximately two minutes long) that was played on a laptop during the session. The content in both interventions was the same however, the media format was different. The session was interactive and participants were encouraged to ask questions as they arose.
Following both interventions, participants were given a post-intervention questionnaire which included qualitative and quantitative evaluation of knowledge domains. Quantitative data was measured using a five-question quiz scored as zero or one, marked out of five. Qualitative data was measured using a five-point Likert scale. Data was collected, and analysed using SPSS 25.0.
Results
The sample consisted of 20 participants in each group (test group and control group) totaling a sample of 40 participants (17 male, 23 female) with ages ranging from 18–83 (mean age 49) (Table 1). Participants were blinded about the study group they were allocated to.
Table 1
| Domains | Group | Mean | Std. error mean | P value |
|---|---|---|---|---|
| Ear anatomy | Animation | 5.00 (SD 0.00) | 0.00 | 0.00 |
| Control | 4.60 (SD 0.50) | 0.11 | ||
| Pathophysiology | Animation | 4.85 (SD 0.37) | 0.08 | 0.02 |
| Control | 4.45 (SD 0.60) | 0.14 | ||
| Pt understanding (symptomatology + treatment) | Animation | 13.95 (SD 1.19) | 0.27 | 0.00 |
| Control | 12.15 (SD 1.87) | 0.42 | ||
| Rating resource | Animation | 14.75 (SD 0.44) | 0.10 | 0.00 |
| Control | 13.60 (SD 1.60) | 0.36 | ||
| Quiz | Animation | 4.80 (SD 0.41) | 0.092 | 0.53 |
| Control | 4.70 (SD 0.57) | 0.13 |
Qualitative results
Cumulative qualitative scores showed a positive difference between the test and control group when looking at pre and post-intervention scores, across all three domains. This included participant understanding of MD (P=0.00), ear anatomy (P=0.00) and pathophysiology of MD (P=0.02) expressing the effectiveness of the 3D animation (Table 1).
Additionally, there was a higher rating of the usefulness of resource in the 3D group in comparison to the control with a statistical significance (P=0.04) (Table 1). Overall, the 3D resources were found to be more effective in improving participants reported understanding of MD (P=0.00) (Table 1), though overall, the value of the difference between the 2 groups was noted to be small.
Quantitative results
This included scores of a knowledge-based quiz which was conducted in addition to the above scores of participants perceptions about their understanding. There was no statistically significant difference in the benefit of the scores between the 2 groups (P=0.53) (Table 1).
Otolaryngologist review results
Otolaryngologists were asked for feedback regarding the animation and their relevant experiences with MD patient education. Results from the questionnaire highlighted that 100% of otolaryngologists determined vertigo to be the most debilitating symptoms and also most likely to impact a patient’s understanding of MD followed by anxiety (70%), hearing loss (30%) and tinnitus (10%) (Table 2).
Table 2
| Question category | Percentage of ENT surgeons | Average score (out of 5) |
|---|---|---|
| Would use tool (rated 3 or more) | 100% | 4 |
| MD symptom impairing to understanding | ||
| Anxiety (rated 4 or more) | 70% | 4 |
| Vertigo | 100% | 5 |
| Tinnitus | 10% | 3 |
| Hearing loss | 30% | 3 |
When addressing the difficulties with MD education, otolaryngologists highlighted areas of difficulty being explaining the complex anatomy and pathophysiology of the inner ear as well as the concept of hydrops in MD pathophysiology and explaining the resulting correlation to their hearing and balance symptoms, which is variable in each patient. Another challenge faced by otolaryngologists was managing the impact that anxiety has on a patient’s understanding of MD. It was exacerbated by the distressing nature of an acute MD attack and unclear aetiology and prognosis. Post-attack, it was identified that the significant debilitating nature of the MD attacks, lack of predictability, risk of drop attacks and the cumulative effects of MD were contributory to ongoing anxiety of MD sufferers. Of concern from the otolaryngologist’s questionnaire, is that patients often seek additional information from alternative sources such as websites, which may be confusing, conflicting or inaccurate. As such, there may be misinformation of sufferers as a result of these resources.
The consensus from the survey of the otolaryngologists is that 100% of the interviewed consultants, liked the animation as they thought it clearly depicted the anatomy and physiology of the inner ear, the concept of hydrops and explained the pathophysiology of MD. Additionally, the otolaryngologists appreciated the relatively short duration of the video (two and a half minutes) and liked that there was no backing audio as they felt that they would be able to tailor information based on the patient’s background level of understanding. otolaryngologists indicated that they would use this 3D animation as part of their education tool inventory.
Discussion
Choice of study content
MD is an area of otolaryngology with complex anatomy (8,9) and pathophysiology (10). In order to understand pathophysiology and disease processes, patient’s needs an understanding of the location of the inner ear, basic inner ear anatomy, audiological and vestibular physiology and then basic concepts of endolymph flow and correlation of hydrops to their symptoms.
MD patients present with a chronic burden on quality of life as a result of the unpredictability of vertiginous attacks and hearing loss (11-13) and may not be able to focus adequately or retain such information (6). Further, patient’s with hearing loss may have added difficulty with verbal cues (6) and as such, visual tools may offer a more suitable aid to understanding for these patients. These symptoms impair communication and may contribute to stress and anxiety that patients already experience by the chronic, debilitating nature of MD (11-13), further influencing control of their MD (12). This is further challenged by the limitation of time during the clinical consultation, information overload while the patient is coming to grips with the impact of the disease on their life as well as ability to recall information discussed. Debilitating symptoms and lack of clarity behind the cause often challenge doctor-patient communication (12) with literature indicating that some MD patients have found their consultation with the GP or otolaryngologist to be ‘unhelpful’ (6). As such, there is a need for alternative tools and adjuncts to assist with improving patient education.
Choice of animation
With multimedia-based educational tools, such as 3D animations, gaining popularity in clinical practice across a variety of disciplines (14-23), it was hypothesised that such medium maybe of value to reduce barriers in doctor patient communication in MD.
An advantage of animation compared to a static picture when dealing with the MD specifically is that it can help with two important challenges: orientation and flow. Firstly, it helps patients unfamiliar with the location of the inner ear, visualise the anatomy of the membranous labyrinth in context of the overall anatomy of the ear, thus orientating the patient. Secondly, it depicts not only normal flow but also the formation and resolution of endolymphatic hydrops throughout the inner ear, thus helping the clinician correlate the patient’s fluctuating auditory and vestibular symptoms with the fluctuating hydrops in the cochlea and/or vestibule or semi-circular canals. Due to the variability in presentation and fluctuation of symptoms of MD which interfaces with the dynamic nature of endolymphatic flow of the inner ear, this cannot be achieved through a static tool such a picture. Lastly, digital tools are free to access by patients, at a time and place convenient to them and this may assist in recall of information and empowers them to discuss this further with their family.
Principal outcome
This study showed that the intervention (3D animation) was effective in positively influencing participants perception of inner ear anatomy, pathophysiology of MD as well as symptomatology and treatment.
Participants from the intervention group (3D animation) reported higher levels of understanding of MD and satisfaction with the educational resource (3D animation) and accordingly, rated the resource higher compared to their control group counterparts. Importantly, the animation was reported to be more engaging by participants than static images, which was also reflected in the otolaryngologist’s questionnaire.
In this study the otolaryngologists all displayed a willingness to use the animation to augment their clinical practice. The results reflected that they felt that barriers in doctor patient communication such as hearing loss, language, health literacy, anxiety, disease specific disability (vertigo and tinnitus) and time limitations can be overcome with using visual based educational resources that augment the clinical interaction. This was echoed further in the study as the clinicians expressed the value of using a 3D tool to explain a 3D concept especially in a disease that often has an unclear aetiology and prognosis with a variable course and presentation.
Limitations of 3D animation study
Although the benefits measured with the animation by participants were statistically significant, the mean difference between the intervention and control group were small. This is most likely attributed to the fact that the sample did not involve Menière’s sufferers. Patients debilitated by the disease and affected by the communication challenges such as hearing loss, anxiety, vertigo identified by the clinicians were more likely to be advantaged by the animation and thus the difference in normal healthy subjects were anticipated to be low. A low sample size (40 participants with 20 in each group) could also be attributed to this. This sample size was calculated and approved by the ethics committee as the minimum sample size that would need to be recruited to show a statistically significant difference.
When objectively testing MD understanding in both groups, there was no statistically significant correlation between self-perceived understanding of MD and the score on the quiz at the end of the session. The possible contributing factors for this include participant comprehension, age (24,25), health literacy (26), and education level (27-31) which were not controlled for. Further, due to logistical issues that would require the participants to be reviewed a second time, retention and recall of information was not tested. It would be of value to add this to future study designs, as the authors feel that this would have been of value to assess.
Strengths
Literature suggests that educational tools, such as 3D animations, have been shown to improve patient comprehension and are more helpful than verbal explanations alone. The results of this study reflected greater participant confidence in their own understanding of MD and their ability to explain this to their family members when using a 3D animation. As such, the 3D animation empowers patients and equips them with the necessary knowledge to understand MD.
It is of significance to note that this entire animation was created by a medical student (second author) as part of his University of Sydney MD project, without any formal training or background in animation. This project was made using free to use software and was created as part of a requirement that arose from a research degree and was created at no cost (Figure 2). The valuable contributions of this research to both doctors and patients depicts a changing topography of a rapidly evolving and highly digitally skilled junior workforce. These skills are worthy of ongoing development in the medical curriculum. In the pedagogy of medicine, knowledge and experience is traditionally passed down from senior to junior colleagues.
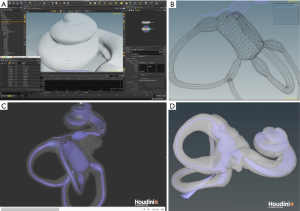
However, in the area of technology literacy and digital learning curve, senior colleagues should actively engage their junior colleagues and medical students in developing such digital educational platform to improve patient care. With further innovation in software development and ease of use, it is likely that such clinically driven platforms will increasingly make it easier for patients to seek reliable and accurate disease specific information.
Conclusions
This study aimed to illustrate and evaluate the effectiveness of a novel 3D animation used for patient education on MD. The results indicated that participants preferred the 3D animation for education and had higher levels of self-reported confidence across all investigated domains of MD. This was also reflected by otolaryngologists who reported benefit in using this tool to overcome barriers in communication with MD patients.
Acknowledgments
The authors acknowledge Dr. Andrew Bradshaw for initially guiding the second author to use the software needed to create the animation. The authors would also like to acknowledge Em Prof. Ian Curthoys and Dr. Chris Wong, who collaborated with A.Prof. Payal Mukherjee to attain the microCT data used in a part of the animation.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CONSORT reporting checklist. Available at http://dx.doi.org/10.21037/ajo-19-71
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ajo-19-71). PM serves as an unpaid editorial board member of Australian Journal of Otolaryngology. JC created the animation creation as part of his MD project at University of Sydney. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The trial was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and the Harmonized Tripartite Guideline for Good Clinical Practice from the International Conference on Harmonization. The study protocol was approved by the Adventist HealthCare Limited Human Research Ethics Committee (2017-044) and was conducted at a single-site at the Sydney Adventist Hospital in the senior author’s ENT clinic. The authors confirm that written informed consent was obtained from the patient for publication of this article and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Yardley L, Kirby S. Evaluation of booklet-based self-management of symptoms in Meniere disease: a randomized controlled trial. Psychosom Med 2006;68:762-9. [Crossref] [PubMed]
- Committee on Hearing and Equilibrium Guidelines for the Diagnosis and Evaluation of Therapy in Meniere's Disease. American Academy of Otolaryngology-Head and Neck Foundation, Inc. Otolaryngol Head Neck Surg 1995;113:181-5. [PubMed]
- Clemmens C, Ruckenstein M. Characteristics of patients with unilateral and bilateral Meniere's disease. Otol Neurotol 2012;33:1266-9. [Crossref] [PubMed]
- Kentala E, Wilson C, Pyykkö I, et al. Positive experiences associated with tinnitus and balance problems. Audiological Medicine 2009;6:55-61. [Crossref]
- Yammine K, Violato C. A meta-analysis of the educational effectiveness of three-dimensional visualization technologies in teaching anatomy. Anat Sci Educ 2015;8:525-38. [Crossref] [PubMed]
- Yardley L, Dibb B, Osborne G. Factors associated with quality of life in Meniere's disease. Clin Otolaryngol Allied Sci 2003;28:436-41. [Crossref] [PubMed]
- Sen P, Papesch M. Ménière Disease Patient Information and Support: Which Website? J Laryngol Otol 2003;117:780-3. [Crossref] [PubMed]
- Mukherjee P, Uzun-Coruhlu H, Curthoys IS, et al. Three-dimensional analysis of the vestibular end organs in relation to the stapes footplate and piston placement. Otol Neurotol 2011;32:367-72. [Crossref] [PubMed]
- Ekdale EG. Comparative Anatomy of the Bony Labyrinth (Inner Ear) of Placental Mammals. PLoS One 2013;8:e66624. [Crossref] [PubMed]
- Vassiliou A, Vlastarakos PV, Maragoudakis P, et al. Meniere's disease: Still a mystery disease with difficult differential diagnosis. Ann Indian Acad Neurol 2011;14:12-8. [Crossref] [PubMed]
- Groen JJ. Psychosomatic Aspects of Menière's Disease. Acta Otolaryngol 1983;95:407-16. [Crossref] [PubMed]
- Orji F. The Influence of Psychological Factors in Meniere's Disease. Ann Med Health Sci Res 2014;4:3-7. [Crossref] [PubMed]
- van Cruijsen N, Jaspers JP, van de Wiel HB, et al. Psychological assessment of patients with Meniere's disease. Int J Audiol 2006;45:496-502. [Crossref] [PubMed]
- Brock TP, Smith SR. Using digital videos displayed on personal digital assistants (PDAs) to enhance patient education in clinical settings. Int J Med Inform 2007;76:829-35. [Crossref] [PubMed]
- Cleeren G, Quirynen M, Ozcelik O, et al. Role of 3D animation in periodontal patient education: a randomized controlled trial. J Clin Periodontol 2014;41:38-45. [Crossref] [PubMed]
- Clements DN, Broadhurst H, Clarke SP, et al. The Effectiveness of 3D Animations to Enhance Understanding of Cranial Cruciate Ligament Rupture. J Vet Med Educ 2013;40:29-34. [Crossref] [PubMed]
- Hermann M. 3-dimensional computer animation--a new medium for supporting patient education before surgery. Acceptance and assessment of patients based on a prospective randomized study--picture versus text. Chirurg 2002;73:500-7. [Crossref] [PubMed]
- Hu J, Yu H, Shao J, et al. An evaluation of the Dental 3D Multimedia System on dentist-patient interactions: A report from China. Int J Med Inform 2008;77:670-8. [Crossref] [PubMed]
- Peltier A, Aoun F, Ameye F, et al. Does Multimedia Education with 3D Animation Impact Quality and Duration of Urologists’ Interactions with their Prostate Cancer Patients? Adv Ther 2015;32:863-73. [Crossref] [PubMed]
- Scherzer J, Buchanan MF, Moore JN, et al. Teaching veterinary obstetrics using three-dimensional animation technology. J Vet Med Educ 2010;37:299-303. [Crossref] [PubMed]
- Schleich JM, Dillenseger JL, Houyel L, et al. A new dynamic 3D virtual methodology for teaching the mechanics of atrial septation as seen in the human heart. Anat Sci Educ 2009;2:69-77. [Crossref] [PubMed]
- Tait AR, Voepel-Lewis T, Chetcuti SJ, et al. Enhancing patient understanding of medical procedures: evaluation of an interactive multimedia program with in-line exercises. Int J Med Inform 2014;83:376-84. [Crossref] [PubMed]
- White SC, Sedler J, Jones TW, et al. Utility of three-dimensional models in resident education on simple and complex intracardiac congenital heart defects. Congenit Heart Dis 2018;13:1045-9. [Crossref] [PubMed]
- Wollinger C, Hirnschall N, Findl O. Computer-based tutorial to enhance the quality and efficiency of the informed-consent process for cataract surgery. J Cataract Refract Surg 2012;38:655-9. [Crossref] [PubMed]
- Tait AR, Voepel-Lewis T, Moscucci M, et al. Patient comprehension of an interactive, computer-based information program for cardiac catheterization: a comparison with standard information. Arch Intern Med 2009;169:1907-14. [Crossref] [PubMed]
- Volk RJ, Jibaja-Weiss ML, Hawley ST, et al. Entertainment education for prostate cancer screening: a randomized trial among primary care patients with low health literacy. Patient Educ Couns 2008;73:482-9. [Crossref] [PubMed]
- Rossi M, McClellan R, Chou L, et al. Informed consent for ankle fracture surgery: patient comprehension of verbal and videotaped information. Foot Ankle Int 2004;25:756-62. [Crossref] [PubMed]
- Bollschweiler E, Apitzsch J, Obliers R, et al. Improving informed consent of surgical patients using a multimedia-based program? Results of a prospective randomized multicenter study of patients before cholecystectomy. Ann Surg 2008;248:205-11. [Crossref] [PubMed]
- Rossi MJ, Guttmann D, MacLennan MJ, et al. Video informed consent improves knee arthroscopy patient comprehension. Arthroscopy 2005;21:739-43. [Crossref] [PubMed]
- Jeste DV, Palmer BW, Golshan S, et al. Multimedia consent for research in people with schizophrenia and normal subjects: a randomized controlled trial. Schizophr Bull 2009;35:719-29. [Crossref] [PubMed]
- Smith OM, McDonald E, Zytaruk N, et al. Rates and determinants of informed consent: a case study of an international thromboprophylaxis trial. J Crit Care 2013;28:28-39. [Crossref] [PubMed]
Cite this article as: John N, Campbell J, Morris S, Mukherjee P. A randomised control trial to evaluate a novel 3D animation for patient education on Menière’s disease. Aust J Otolaryngol 2020;3:18.


