
Argon plasma coagulation versus cold steel tonsillectomy: a comparison of safety and efficacy
Introduction
Tonsillectomy is one of the most commonly performed procedures in otolaryngology worldwide. Various techniques have been introduced as alternatives to cold steel (CS) dissection in search for better techniques with reduced morbidity. There is no conclusive evidence in the literature as to which surgical technique is best for tonsillectomy (1-4).
Application of Argon plasma coagulation (APC) in tonsillectomy was first described by Bergler et al. (5) in 2000. This technique utilises a high-frequency current to ionise argon gas, creating an argon plasma field that is transmitted to the tissue surface in a non-contact fashion. The argon plasma field is conducted to the target tissue via the path of least resistance, diverting away from areas already coagulated. APC has been shown to achieve homogenous haemostasis and limited depth of penetration, with minimal damage to surrounding tissues (5,6).
There appears to be a paucity of large, recent comparative studies on the use of APC tonsillectomy. Only five studies (5,7-10) have directly compared outcomes of APC with CS tonsillectomy in the medical literature, most recent being Ferri and Armato (8) in 2011. Of these, only two studies included data in the paediatric cohort, specifically in young children and infants (7,8). None of the five studies were based on single-surgeon experience. The largest cohort thus far was in a study by Ferri et al. (9), which involved 226 adult patients. The authors present the largest single-surgeon comparative study in the medical literature, involving both adult and paediatric patients, on APC versus CS tonsillectomy.
The aim of this study was to compare safety and efficacy of APC with CS dissection in tonsillectomy, by evaluating the following parameters: (I) operative time; (II) intraoperative haemorrhage; (III) postoperative pain and (IV) postoperative primary and secondary haemorrhage.
Methods
Patients
This was a retrospective analysis of a prospectively collected database, conducted in Adelaide, South Australia. We identified all patients who underwent elective bilateral tonsillectomies performed by the senior author (CK Shaw) over a period of 5 years across multiple local institutions. Patients were excluded if they had a known bleeding diathesis, took anticoagulants or non-steroidal anti-inflammatory medications (NSAIDs) within 10 days of their operation, or underwent concurrent other oral or oropharyngeal procedures. A total of 500 patients were included in this study, of which APC group accounted for 232 patients and CS group 268 patients.
All patients received standard counselling during preoperative consultations with their surgeon (CK Shaw). Patients were not advised which technique would be used at the time of surgery as both techniques have been shown to be safe (5,7-10). The choice between APC and CS tonsillectomy was based on the availability APC equipment at the local institution.
This study was approved by the local Human Research Ethics Committee.
Equipment
The ExplorAr® ST700-311EI electrode (ConMed Linvatec Australia PTY Ltd.) with a 10-mm medium Tungsten needle and a 5-mm extension with insulation was used in all APC tonsillectomies. This was a single-use, disposable electrode with a fine dissection tip, which differs considerably from the Bergler’s Dissector, as used in all other APC studies (5,7-10). In our experience, the fine electrode tip allows for excellent precision and better control during dissection. The electrode is attached to a System 7550™ Generator Unit and a “Size D” Argon Supply Tank (CONMED Linvatec Australia PTY Ltd.). The generator was set at 20 Watts and argon gas flow rate was set at 4.0 standard litres per minute. It has been shown that at 40 Watts APC produces a depth of injury of 0.19 mm at 1 second, and 0.82 mm at 5 seconds (6). Depth of injury can be further controlled by increasing or decreasing the speed of application.
Operative technique
All patients underwent tonsillectomies with standard perioperative care. All cases were performed under general anaesthesia, with endotracheal intubation, Boyle-Davis gag and an intraoperative dose of intravenous dexamethasone. No patient received prophylactic antibiotics. All tonsillectomies were performed by a single surgeon (CK Shaw). Techniques for APC and CS tonsillectomy were standardized and uniform.
APC tonsillectomy was performed as follows. Superior pole of the tonsil was grasped with forceps. Anterior pillar was dissected under continuous activation of the APC electrode, in a one-step coagulation and dissection process, in a non-contact fashion. The tonsil was dissected from the tonsillar fossa until lower pole of the tonsil is reached and removed. In cases of intensive vascularisation, the speed of dissection was reduced to allow sufficient coagulation. Bipolar coagulation was used in cases of large visible vessel or brisk bleeding.
CS tonsillectomy was performed in the usual manner using Gwynne Evans Dissector and silk ties to inferior stalk. Tonsillar fossa was packed with gauze swabs and bipolar coagulation was used to achieve complete haemostasis.
Postoperative management
Patients were discharged on day 1 with follow-up arranged at 3 weeks. All patients were put on a standard regimen of regular paracetamol for 7 days; with or without benzydamine gargle and opioid analgesia as required. They were instructed not to take NSAIDs and not prescribed steroids on discharge. Patients were encouraged to fill out a pain score chart for the first 14 postoperative days and return this upon follow-up.
Outcomes
Four outcomes measures were identified in this study:
- Operative time was defined as time (minutes, seconds) from insertion of Boyle-Davis gag to time at complete haemostasis after gag release, as measured by a timer.
- Intraoperative blood loss was evaluated in a categorical fashion, using a classification system for assessing the severity of blood loss (Table 1). A grade was assigned to each case intraoperatively by the surgeon, taking into account the amount of blood lost (mL) in the suction canister, the nearest whole number of soaked gauze swabs, and use of additional measures to achieve haemodynamic stability, if any. Prior to this study, a simple experiment was conducted to determine the amount of blood required to soak 1 swab (Zhen and Shaw, unpublished data, 2018). Corresponding volumes (mL) were calculated for each grade so that it may be comparable to other studies.
- Postoperative pain was evaluated on a 10-point Visual Analogue Scale (VAS), with 0 being “no pain” and 10 being “worse pain possible”, over a period of 14 days, in patients aged 5 and above. VAS is a validated method for assessment of acute, subjective pain in older children and adults (11-13). Pain scores from patients below 5 years of age were not included in this study, based on evidence that children 0–4 years of age are less likely to self-report pain scores, and that administration of rescue analgesics is affected by parental assessment and anxiety (14-16).
- Postoperative haemorrhage was defined as either primary, where bleeding occurred within the first 24 hours of surgery, or secondary, where bleeding occurred after the first 24 hours. The number of postoperative haemorrhage events in each group was recorded. The severity of each event was then stratified based on a 7-grade classification of post-tonsillectomy haemorrhage adapted from Sarny et al. (17) (Table 2).
Table 1
| Grade | Clinical finding |
|---|---|
| Grade 1 | No or minimal bleeding |
| 1a | Zero to 1 soaked gauze swab, and no blood in the suction canister |
| 1b | Zero to 1 soaked gauze swab, and 0–10 mL in the suction canister |
| Grade 2 | Mild bleeding: between 1–5 soaked gauze swabsϮ, and 11–50 mL in the suction canister |
| Grade 3 | Moderate bleeding: between 5–10 soaked gauze swabsϮ, and 51–100 mL in the suction canister |
| Grade 4 | Moderately severe bleeding: between 10–15 soaked gauze swabsϮ, and 101–200 mL in the suction canister |
| Grade 5 | Severe bleeding: |
| Any amount of blood loss exceeding grade 4, or | |
| Perioperative blood transfusion, or | |
| Ligation of the external carotid artery |
*, an experiment was conducted by the authors to measure amount of blood required to completely soak 1 standard gauze swab of 7.5 cm × 7.5 cm (Zhen and Shaw, unpublished data, 2018). Based on the finding that each swab soaks up approximately 5 mL, corresponding volumes (mL) for each grade are as follows: grade 1a =0–5 mL, mean 2.5 mL; grade 1b =6–15 mL, mean 7.5 mL; grade 2 =16–75 mL, mean 45.5 mL; grade 3 =76–150 mL, mean 113 mL; grade 4 =151–275 mL, mean 213 mL; grade 5 = >275 mL. Ϯ, rounded to the nearest whole number of soaked swabs.
Table 2
| Grade | Clinical finding |
|---|---|
| Grade A | Blood-tinged sputum, no intervention |
| A1 | Dry wound, no coagulum |
| A2 | Coagulum evident, dry wound after removal |
| Grade B | Bleeding actively upon examination, minimal interventions at bedside |
| B1 | Bleeding stopped with non-invasive treatment (e.g., adrenalin sponge) |
| B2 | Bleeding stopped with treatment under local anaesthesia |
| Grade C | Return to theatre, no haemodynamic instability |
| Grade D | Return to theatre, blood transfusion required |
| Grade E | Fatal haemorrhage |
*, adapted with permission from “Classification of Postoperative Bleeding Episodes” by Sarny et al. (17).
Statistical analysis
Data was analysed using GraphPad Prism version 6.00 (GraphPad Software, La Jolla California USA, www.graphpad.com). A P value of less than 0.05 was considered statistically significant. Statistical analysis for operative time was analysed using a two-tailed Student’s t-test. Postoperative pain scores were analysed in two ways: mean daily pain scores (days 1–14) were compared between the two groups using a paired Student’s t-test; mean total pain scores were compared using an unpaired Student’s t-test. Intraoperative and postoperative haemorrhage grades were analysed using the Chi square test.
Results
A total of 500 patients were included in this study. Patient demographics between the two groups were compatible (Table 3).
Table 3
| Variables | APC group (n=232) | CS group (n=268) | Study cohort (n=500) |
|---|---|---|---|
| Age, years | |||
| Median | 9 | 7 | 7 |
| Range | 1–46 | 1–57 | 1–57 |
| Sex | |||
| Male (%) | 41.38 | 39.67 | 40.50 |
| Female (%) | 58.62 | 60.33 | 59.49 |
| Male/female ratio | 0.71 | 0.66 | 0.68 |
APC, Argon plasma coagulation; CS, cold steel.
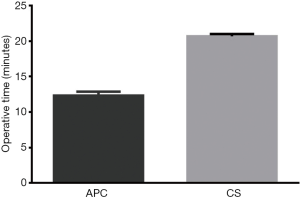
Operative time was compared between the two groups (Figure 1). Mean duration was 12.33 minutes [standard deviation (SD) 0.284] for APC group and 20.68 minutes (SD 0.16) for CS group. Difference between the means was 8.354 minutes (SD 0.326, 95% CI: 7.712–8.996) in favour of APC group (P<0.001).
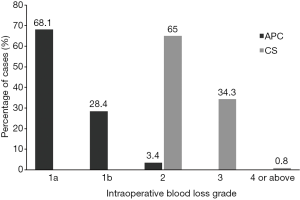
Intraoperative blood loss was classified into 7 grades (Table 1) and the number of cases in each grade was analysed using the Chi square test. The results showed a significant reduction in intraoperative blood loss in APC group compared to CS (χ24=187.5, P<0.001) (Figure 2). The majority of cases in APC group had no or minimal blood loss, in contrast to mild to moderate blood loss for the majority of CS group. Additionally, two cases of grade 4 blood loss occurred in CS group. No patient in this study required blood transfusion or ligation of the external carotid artery.
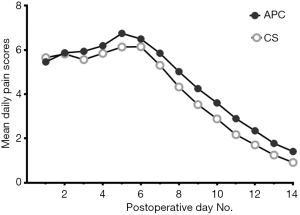
Pain score charts from 135 patients were not returned on follow-up and charts from patients below 5 years of age were excluded. Thus, for analysis of postoperative pain, the number of subjects available were 107 in APC group and 98 in CS group. Analysis of mean daily pain scores revealed that the two groups had similar pain profiles (Figure 3). With exception to day 1, CS group had consistently lower pain scores than APC, with difference of the means being 0.47 (SD 0.27, 95% CI: 0.31–0.63, P<0.001). Mean total pain scores were calculated to reflect the overall pain experience for each group, which were 4.54 and 4.09 for APC and CS groups, respectively. The difference between the means was 0.45 of a pain score (SD 0.22, 95% CI: 0.02–0.88, P=0.04), consistent with the previous analysis.
There were no cases of primary postoperative haemorrhage in this study (Table 4). A total of 23 secondary haemorrhage events occurred, of which APC group accounted for 9 and CS accounted for 14. Incidence of secondary haemorrhage appeared to be lower in APC group than CS group. Most of these events were blood-tinged sputum not requiring intervention and only two cases required return to theatre. These two cases occurred in paediatric patients (16-year-old and 9-year-old), which could reflect a lower threshold for early surgical management of post tonsillectomy bleeding in children. We were unable to demonstrate a statistical difference between the two groups in incidence or severity due to inadequate sample size (χ22=3.7, P=0.16).
Table 4
| Variables | APC group (n=232) | CS group (n=268) | Study cohort (n=500) |
|---|---|---|---|
| Primary haemorrhage, n | 0 | 0 | 0 |
| Secondary haemorrhage, n (%) | 9 (3.88) | 14 (5.22) | 23 (4.60) |
| Grade, n | |||
| A1 | 6 | 13 | 19 |
| A2 | 1 | 1 | 2 |
| B1–B2 | 0 | 0 | 0 |
| C | 2 | 0 | 2 |
| D–E | 0 | 0 | 0 |
| Postoperative days, range | 4–10 | 4–9 | 4–10 |
Grade A1 = blood-tinged sputum with dry wound, no coagulum; grade A2 = blood-tinged sputum with coagulum, dry wound after removal; grade B1 = bleeding actively upon examination, stops with non-invasive treatment; grade B2 = bleeding actively under examination, stops with treatment under local anaesthesia; grade C = return to theatre, no haemodynamic instability; grade D = return to theatre and required blood transfusion; grade E = fatal haemorrhage. APC, Argon plasma coagulation; CS, cold steel.
Discussion
Outcome measures
In this study, we found a significant reduction in operative time by an average of 8.354 minutes (95% CI: 7.712–8.996), and minimal intraoperative blood loss in the APC group, consistent with current literature (5,7-10). Ferri and Armato (8) quoted intraoperative blood loss of 6.4 mL with APC versus 48.12 mL with CS in a paediatric cohort. Our findings were similar. The majority of APC cases had grade 1a blood loss, equivalent to 0–2 mL, and the majority of CS cases had grade 2 blood loss, equivalent to 14–65 mL.
The APC group had slightly higher postoperative pain scores, with a difference of 0.45 in mean pain scores compared to CS. This is comparable to findings of other APC/CS studies, where differences in postoperative pain scores did not amount to statistical significance (5,7-10). According to a study by Lee et al. (18) on minimum clinically important difference (MCID) for VAS, the MCID was 30 in a 100-point VAS for adults, which correlated to the point at which there was perceived inadequate analgesic control, and 72.5 the point at which patients requested parenteral analgesics. Correspondingly, the MCID in our study should be 3. Therefore, a 0.45 difference in pain scores is unlikely to represent any perceivable difference in pain between the APC and CS groups, and very unlikely to represent clinically significant pain issues requiring admission for analgesia or steroids. Additionally, we found that APC and CS groups had similar pain profiles over the initial 14 days, without evidence of a delayed peak in pain as described by Skinner et al. (10). It would be reasonable, therefore, to advise patients that their pain experience would be the same as a “cold” tonsillectomy.
In our study, APC technique did not result in increased primary haemorrhage, which reflects adequate intraoperative haemostasis (19). The rate of secondary haemorrhage in the literature is difficult to evaluate, as methods for reporting postoperative haemorrhage vary considerably from study to study (17,19,20). In this study, secondary haemorrhage occurred in 4.6% of cases, and 0.2% required return to theatre. Our rates were considerably lower than those quoted in a large study by Sarny et al. (17), which were 15% for secondary haemorrhage and 4.6% for return to theatre, using the same post-tonsillectomy haemorrhage classification (Table 2). Studies such as ours invariably present an overestimate of secondary haemorrhage in clinical practice, as all incidents of blood-tinged sputum, even those without evidence of active bleeding, are recorded as a positive event. Therefore, at a glance, our rates of secondary haemorrhage may appear higher than other studies.
Safety and efficacy of APC
It is well established that “Hot” techniques are known to shorten operative time, as a result of the one-step dissection and coagulation nature of electrosurgery (1). Concerns with electrosurgery have traditionally been related to increased postoperative pain due to increased local inflammation and oedema and increased postoperative haemorrhage due to collateral thermal injury and tissue necrosis (1,3,21). These issues affect the safety of techniques such as diathermy and coblation (1,3,22).
APC may be an improvement upon other techniques in this regard. Its depth of penetration is limited and can be controlled by titrating the electrical voltage and varying the speed of application, resulting in a thinner eschar. This may explain the apparent reduction in secondary haemorrhage, as sloughing of eschar from the tonsillar fossa has been implicated in the etiology of post-tonsillectomy bleeding (19). This presents a significant advantage for APC tonsillectomy over electrosurgical techniques associated with increased secondary haemorrhage.
The reduction in intraoperative bleeding in APC tonsillectomy is particularly meaningful for paediatric patients, as they are placed at greater risk of haemodynamic instability compared to adults. A “bloodless” technique also has inherent benefits for patients with underlying bleeding diathesis, and those with religious objections to blood transfusions.
There are several other advantages of APC tonsillectomy worth noting. Firstly, APC is able to provide a clear dissection plane as the argon gas jet pushes blood and debris aside. This is helpful in paediatric tonsillectomy, where the surgical field is limited, and patients with a past history of peritonsillar abscess, where dissection plane can be poorly demarcated. Secondly, unlike laser, special personal protective equipment is not required for patients or staff and no additional safety training is required for theatre personnel. Lastly, APC tonsillectomy appears to be cheaper compared to some of the other tonsillectomy techniques on offer. CS would always be cheapest as it does not require any handpiece or additional equipment, and instruments can be reused by sterilisation. However, APC greatly reduces operative time and may result in improved theatre utilization. The cost of an ExplorAr® ST700-311EI electrode is AUD $76.50 and a standard size Argon Gas Tank will last between 4 to 6 months. In comparison, at our institution, a single-use BiZact™ handpiece cost AUD $270 and coblation AUD $380. A cost-benefit analysis is needed to investigate which technique is most economical.
We acknowledge several limitations with this study. Firstly, this was not a prospective study despite deriving our conclusions from a prospectively collected database. Patients were not randomly assigned to APC and CS groups; therefore, a degree of selection bias exists depending on where patients were arranged to have surgery. However, demographics analysis demonstrated similar baseline characteristics between the two groups. Secondly, intraoperative blood loss was evaluated using a categorical system, based on a combination of estimated volume loss and rescue measures taken to achieve haemostasis, instead of being directly reported in “mL”. This method was chosen because we recognise that there is always an inherent degree of inaccuracy in the measurement of intraoperative blood loss. Small volumes lost in the tubing of suction canisters and drying of gauze swabs render measuring and weighing methods impractical. Unaccounted volumes can be significant if total blood loss is minimal, as is the case with APC. Therefore, a categorical assessment of intraoperative blood loss was used. Thirdly, our findings are based on the outcomes of a single, experienced ear, nose and throat (ENT) surgeon who is proficient in the use of APC. Surgical outcomes may be variable for those less experienced with this technique. Lastly, our sample size was not large enough to demonstrate a meaningful difference in postoperative haemorrhage. Larger studies sufficiently powered to investigate postoperative haemorrhage rate in APC tonsillectomy are needed.
Conclusions
APC appears to be a safe and efficacious technique for tonsillectomy in both adults and children. It has the advantage of reduced operative time, less intraoperative bleeding and similar postoperative pain experience compared to CS tonsillectomy. Further studies are needed to further investigate its rate of post-tonsillectomy haemorrhage and cost-effectiveness.
Acknowledgments
The authors thank Dr Joshua Jervis-Bardy (MBBS, PhD, FRACS), for assistance in manuscript preparation and Dale Mackay, ConMed Linvatec Australia PTY Ltd., for providing APC product specifications.
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ajo.2019.09.02). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the local Human Research Ethics Committee (No. HREC/13/TQEHLMH/69). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Informed consent was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Blanchford H, Lowe D. Cold versus hot tonsillectomy: state of the art and recommendations. ORL J Otorhinolaryngol Relat Spec 2013;75:136-141. [Crossref] [PubMed]
- Alexiou VG, Salazar-Salvia MS, Jervis PN, et al. Modern technology-assisted vs conentional tonsillectomy: a meta-analysis of randomized controlled trials. Arch Otolaryngol Head Neck Surg 2011;137:558-70. [Crossref] [PubMed]
- Burton MJ, Doree C. Coblation versus other surgical techniques for tonsillectomy. Cochrane Database Syst Rev 2007;CD004619. [PubMed]
- Pinder DK, Wilson H, Hilton MP. Dissection versus diathermy for tonsillectomy. Cochrane Database Syst Rev 2011;CD002211. [PubMed]
- Bergler W, Huber K, Hammerschmitt N, et al. Tonsillectomy with the argon-plasma-coagulation-raspatorium - a prospective randomized single-blinded study. HNO 2000;48:135-41. [Crossref] [PubMed]
- Canady J, Wiley K, Ravo B. Argon Plasma Coagulation and the Future Applications for Dual-Mode Endoscopic Probes. Rev Gastroenterol Disord 2006;6:1-12. [PubMed]
- Bergler W, Huber K, Hammerschmitt N, et al. Tonsillectomy with argon plasma coagulation (APC): evaluation of pain and hemorrhage. Laryngoscope 2001;111:1423-9. [Crossref] [PubMed]
- Ferri E, Armato E. Argon plasma coagulation versus cold dissection in pediatric tonsillectomy. Am J Otolaryngol 2011;32:459-63. [Crossref] [PubMed]
- Ferri E, Armato E, Capuzzo P. Argon plasma coagulation versus cold dissection tonsillectomy in adults: a clinical prospective randomized study. Am J Otolaryngol 2007;28:384-7. [Crossref] [PubMed]
- Skinner LJ, Colreavy MP, Lang E, et al. Randomized controlled trial comparing argon plasma coagulation tonsillectomy with conventional techniques. J Laryngol Otol 2003;117:298-301. [Crossref] [PubMed]
- American Academy of Pediatrics. Committee on Psychosocial Aspects of Child and Family Health; Task Force on Pain in Infants, Children, and Adolescents. The assessment and management of acute pain in infants, children, and adolescents. Pediatrics 2001;108:793-7. [PubMed]
- Revill SI, Robinson JO, Rosen M, et al. The reliability of a linear analogue for evaluating pain. Anaesthesia 1976;31:1191-8. [Crossref] [PubMed]
- Breivik H, Borchgrevink PC, Allen SM, et al. Assessment of pain. Br J Anaesth 2008;101:17-24. [Crossref] [PubMed]
- Boelen-van der Loo WJ, Scheffer E, de Haan RJ, et al. Clinimetric evaluation of the pain observation scale of young children aged between 1 and 4 years after ear, nose, and throat surgery. J Dev Behav Pediatr 1999;20:222-7. [Crossref] [PubMed]
- de Jong AE, Bremer M, Schouten M, et al. Reliability and validity of the pain observation scale for young children and the visual analogue scale in children with burns. Burns 2005;31:198-204. [Crossref] [PubMed]
- Chambers CT, Finley GA, McGrath PJ, et al. The parents' postoperative pain measure: replication and extension to 2-6-year-old children. Pain 2003;105:437-43. [Crossref] [PubMed]
- Sarny S, Ossimitz G, Habermann W, et al. Haemorrhage following tonsil surgery: a multicenter prospective study. Laryngoscope 2011;121:2553-60. [Crossref] [PubMed]
- Lee JS, Hobden E, Stiell IG, et al. Clinically important change in the visual analog scale after adequate pain control. Acad Emerg Med 2003;10:1128-30. [Crossref] [PubMed]
- Milobević DN. Intensity of hemorrhage following tonsillectomy. Vojnosanit Pregl 2012;69:500-3. [Crossref] [PubMed]
- Subramanyam R, Varughese A, Willging JP, et al. Future of pediatric tonsillectomy and perioperative outcomes. Int J Pediatr Otorhinolaryngol 2013;77:194-9. [Crossref] [PubMed]
- Lowe D, van der Meulen JNational Prospective Tonsillectomy Audit. Tonsillectomy technique as a risk factor for postoperative haemorrhage. Lancet 2004;364:697-702. [Crossref] [PubMed]
- Lowe D, Cromwell DA, Lewsey JD, et al. Diathermy power settings as a risk factor for hemorrhage after tonsillectomy. Otolaryngol Head Neck Surg 2009;140:23-8. [Crossref] [PubMed]
Cite this article as: Zhen E, Shaw CKL. Argon plasma coagulation versus cold steel tonsillectomy: a comparison of safety and efficacy. Aust J Otolaryngol 2019;2:25.


