
The suspended endoscopy technique (SET) for intra-operative assessment in awake type I thyroplasty—how I do it
Introduction
Thyroplasty has been increasingly utilized as a technique to treat glottic insufficiency over the last 20 to 30 years (1). Although its roots can be traced back as early as 1911, when Brunnings documented one of the first attempts to repair vocal cord palsy, the difficulties in ensuring safety and short- and long-term efficacy of the procedure has led to its variable popularity in the past (2). It was only in 1974 when Isshiki and associates described what is now known as type I thyroplasty that the concept truly gained traction (3). Although the concept of inducing external medialisation of the vocal cord had been previously proposed by Payr in 1915 (2), unpredictability in the degree of vocal fold displacement had meant that this technique had been largely superseded by percutaneous injection techniques. Percutaneous techniques, however, were predominantly temporary therapies, and also had their complications, including foreign body reactions and granuloma formation (4,5).
The original technique as outlined by Isshiki and associates involved creating a window in the anterior thyroid cartilage ala under local anaesthetic and inserting a silicon implant into the paraglottic space, ensuring preservation of the perichondrium. Since that time, there have been various modifications, including the use of Gore-Tex strips (stretched polytetrafluoroethylene. W.L. Gore and Associates, Inc., Flagstaff, AZ, USA) to allow for a more dynamic and fine-tuned medialisation, and the combination with other phonosurgical techniques, such as arytenoid adduction and reinnervation procedures (2). Aside from providing real-time adjustable medialisation (compared with silicone implants which either come pre-moulded or require intra-operative moulding), Gore-Tex strips have the advantage of delivering both anterior and posterior medialization with a smaller thyrotomy window.
Traditionally, phonological feedback has been the predominant method of determining the degree of medialisation provided. However, this is often influenced by localised oedema and blood which makes estimation of medialisation difficult and creates undesirable post-operative glottic insufficiency following oedema resolution. The introduction of flexible fibreoptic or video-nasendoscopy has allowed for inspection of the larynx and vocal fold alignment prior to procedure, and confirmation of vocal fold alignment at the conclusion and at time of follow-up. This requires an extra assistant to position the scope, and hold it in place for the duration of Gore-Tex insertion to assess the degree of medialisation provided. Combined with phonatory feedback, functional and anatomical optimisation can be achieved and potential complications reduced.
Methods
A modification to the technique of awake type I thyroplasty is described, which allows for the entire procedure to be performed by a single operator, with both phonological and visual endoscopic feedback throughout the entire case.
The patient is laid supine at the commencement of the procedure and co-phenylcaine applied to the nasal passages and throat for nasal decongestion and topical anaesthesia of the nasal cavity and larynx. A flexible fibreoptic nasendoscope is then positioned in place with optimal view of the larynx and vocal cords, and suspended about an overhanging hook and fastened securely with a firm holding clip (Figures 1,2), or even a cable tie so as to not allow for accidental release from its suspended position and avoid harm to the patient. The nasendoscope should be suspended at a height just above the supraglottis, avoiding irritation and induction of the cough or gag reflex. The lead of the nasendoscope is inserted into a camera stack placed across from the surgeon. A top drape is suspended from two drip stands to separate the sterile field from the non-sterile field. The operator can then undergo surgical scrub for the duration of the procedure.


Following initial setup and preparation of the incision site, a window is created in the anterior thyroid cartilage under local anaesthetic. Gore-Tex strips are inserted with continuous phonatory and endoscopic visual feedback. Vocal fold alignment is then checked prior to concluding the procedure.
Other adjuncts to this technique include the use of a nasopharyngeal airway to assist nasendoscope passage, as well as a simple Hudson mask with a small window fashioned (to allow for entry of the scope) for patients who may require intraoperative oxygen supplementation (Figure 3).

Patients also receive speech therapy before and after the procedure, to reduce secondary muscle tension dysphonia (supraglottic compensatory hyperfunction).
This method of type I thyroplasty was adopted in 10 pilot cases over the course of 1 year at our institution (Westmead Hospital, Sydney, Australia). Patients were initially reviewed in voice clinic with flexible fibreoptic nasendoscope and strobe to confirm the presence of unilateral vocal cord palsy. Patients were deemed suitable for trial of the suspended endoscopy technique (SET) if they were able to tolerate fibreoptic nasoendoscopic examination in clinic, and if they were considered to be able to lie still for the duration of procedure. All patients who met this criterion in the 1-year period were included in the trial. Standard parameters for type I Thyroplasty, including patient age, gender, duration of vocal cord palsy, cause of vocal cord palsy and presence of prior vocal cord injection were obtained. Maximal phonatory time (MPT) was also recorded by measuring the longest duration a vowel sound could be sustained on serial testing (three times). Laryngeal EMG was used to confirm absence of vocal cord neuromuscular activity in some cases, but was not used in cases where the clinical likelihood of nerve palsy was high, or where the procedure was done for palliation (e.g., lung carcinoma).
Intra-operative complications including poor patient tolerance of the fibreoptic nasendoscope, dislodgement of and damage to the scope were specifically sought after.
Patients were reviewed again in voice clinic 3 months post-operatively for repeat MPT measurement to assess efficacy of procedure. Need for revision surgery was also recorded.
Results
In the 10 pilot cases performed at this institution, this technique has been found to be safe and efficient. No complications or unanticipated events have been noted.
Results are presented in Table 1.
Table 1
| Case number | Gender | Age (years) | Duration of vocal cord palsy (months) | Cause | Injection prior | Laryngeal EMG | Supraglottal hyperfunction (pre-op) | Pre-op MPT (seconds) | Post-op MPT (seconds) | Revision required? | Follow-up duration (months) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 63 | 12 | Post-thyroidectomy | Yes | Yes | Yes | 3 | 13 | No | 12 |
| 2 | F | 72 | 9 | Post-thyroidectomy | Yes | Yes | Yes | 5 | 17 | No | 9 |
| 3 | F | 75 | 15 | Lung carcinoma | No | No | No | 3 | 11 | No | 15 |
| 4 | F | 52 | 15 | Intubation | No | Yes | Yes | 4 | 11 | No | 12 |
| 5 | F | 47 | 10 | Idiopathic | Yes | Yes | Yes | 7 | 16 | No | 10 |
| 6 | M | 71 | 11 | Skull base tumour | No | No | No | 5 | 14 | No | 3 |
| 7 | M | 68 | 12 | Skull base tumour | No | No | No | 5 | 16 | No | 7 |
| 8 | M | 61 | 15 | Post-thyroidectomy | Yes | Yes | Yes | 4 | 16 | No | 4 |
| 9 | F | 58 | 18 | Post-thyroidectomy | Yes | No | Yes | 4 | 15 | No | 18 |
| 10 | F | 53 | 12 | Lung carcinoma | No | No | No | 3 | 11 | No | 12 |
MPT, maximal phonatory time.
The post-op mean MPT was 14 s, compared with a pre-op mean of 4.3 s. No cases required revision surgery at time of last follow-up.
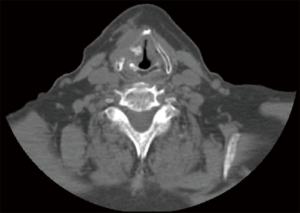
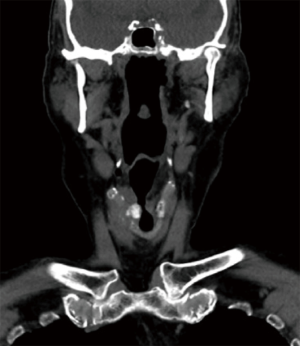
Figures 4 and 5 demonstrate radiological evidence of optimal Gore-Tex placement following our technique of type I thyroplasty.
Discussion
Flexible fibreoptic nasendoscopy was introduced to thyroplasty as a method for examining the larynx and assessing vocal fold position prior to procedure, and for confirming position post-implantation. There are significant benefits conferred by using endoscopy intra-operatively: visual feedback of vocal fold position during the procedure allows for adjustment of Gore-Tex placement, and overcomes the erroneous estimation of medialisation from using phonological feedback alone.
The main advantage of the SET over previous methods is the continuous visual endoscopic feedback provided throughout the procedure without the need for an additional assistant trained in flexible nasendoscope placement. This is important in settings where the surgeon is the sole operator, as is common in many private arrangements, or in under-resourced areas and peripheral hospitals. Furthermore, visual feedback throughout the case allows for prevention of overuse of implant material and incorrect placement which can lead to implant extrusion, partial airway obstruction and breathing difficulties (6,7). Complications such as haematomas can also be detected early.
In practice, no events of scope dislodgement or damage to the nasendoscope when suspended in this manner have been noted.
The procedure requires a compliant patient who can remain still for the duration of the case and tolerate a nasendoscope in situ. Careful patient selection is thus important, and there have been no issues with patient tolerance noted so far.
This technique offers a convenient adjunct to the current method of type I thyroplasty. It is of low cost, and utilizes instruments and resources which are already readily available in most ENT departments. Although not the focus of this paper, the results of the parameters tested show that this technique is effective (mean improvement in MPT 9.7 s) and comparable to previously published data on voice post standard type I thyroplasty (8-10), with no additional complications.
Conclusions
We recommend that the SET may be used for intra-operative assessment for routine awake type I thyroplasty.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ajo.2018.05.04). FR serves as an unpaid editorial board member of Australian Journal of Otolaryngology. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Informed consent was taken from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Mallur PS, Rosen CA. Vocal fold injection: review of indications, techniques, and materials for augmentation. Clin Exp Otorhinolaryngol 2010;3:177-82. [Crossref] [PubMed]
- Crolley VE, Gibbins N. One hundred years of external approach medialisation thyroplasty. J Laryngol Otol 2017;131:202-8. [Crossref] [PubMed]
- Isshiki N, Morita H, Okamura H, et al. Thyroplasty as a new phonosurgical technique. Acta Otolaryngol 1974;78:451-7. [Crossref] [PubMed]
- Netterville JL, Coleman JR Jr, Chang S, et al. Lateral laryngotomy for the removal of Teflon granuloma. Ann Otol Rhinol Laryngol 1998;107:735-44. [Crossref] [PubMed]
- Kirchner FR, Toledo PS, Svoboda DJ. Studies of the larynx after teflon injection. Arch Otolaryngol 1966;83:350-4. [Crossref] [PubMed]
- Weinman EC, Maragos NE. Airway compromise in thyroplasty surgery. Laryngoscope 2000;110:1082-5. [Crossref] [PubMed]
- Abraham MT, Gonen M, Kraus DH. Complications of type I thyroplasty and arytenoid adduction. Laryngoscope 2001;111:1322-9. [Crossref] [PubMed]
- Chowdhury K, Saha S, Saha VP, et al. Pre and post operative voice analysis after medialization thyroplasty in cases of unilateral vocal fold paralysis. Indian J Otolaryngol Head Neck Surg 2013;65:354-7. [Crossref] [PubMed]
- Rzepakowska A, Osuch-Wojcikiewicz E, Sielska-Badurek E, et al. Medialization thyroplasty in glottis insufficiency due to unilateral vocal fold paralysis and after laser cordectomies - preliminary report. Otolaryngol Pol 2017;71:22-9. [Crossref] [PubMed]
- Elnashar I, El-Anwar M, Amer H, et al. Voice Outcome after Gore-Tex Medialization Thyroplasty. Int Arch Otorhinolaryngol 2015;19:248-54. [Crossref] [PubMed]
Cite this article as: Lau J, Loizou P, Palme C, Riffat F. The suspended endoscopy technique (SET) for intra-operative assessment in awake type I thyroplasty—how I do it. Aust J Otolaryngol 2018;1:15.


