
How I do it: modification of the posterior pedicled nasoseptal flap for clival and nasopharyngeal surgery
Introduction
The posterior pedicle nasoseptal flap, also named the Hadad-Bassagaisteguy flap, was developed at the University of Rosario, Argentina by Hadad and Bassagaisteguy, and modified by Carrau with the aim to design a better intranasal vascular pedicled flap for skull base reconstruction (1,2). The posterior pedicle nasoseptal flap provides an ample surface area with a superior arc of rotation and is therefore a reliable flap, especially for the reconstruction of large skull base defects. Due to the length of its pedicle, this flap may be used to reconstruct defects resulting from an approach or resection involving the cribriform plate, a sellar or suprasellar lesion, the planum sphenoidale or clivus (2). Anteriorly, its surface area is enough to cover a defect that spans the anterior cranial fossa from orbit to orbit and from the frontal sinus to the planum sphenoidale. Posteriorly it can cover a panclivectomy (i.e., from the posterior clinoids superiorly to the foramen magnum inferiorly) (3).
One of the limitations of the posterior pedicle nasoseptal flap is that it must be harvested at the beginning of surgery, prior to the posterior septectomy and before the final dimensions of the skull base defect are known; therefore, its use requires forethought and planning. Subsequently, the flap dimensions must be overestimated.
Once harvested, the posterior pedicle nasoseptal flap is commonly stored in the nasopharynx or inside the maxillary or sphenoid sinus to avoid injury during extirpative surgery. However, these sites are not always ideal. Placing the nasoseptal flap in these locations often results in significant venous congestion of the flap, risking its viability. Furthermore, placing the flap in the nasopharynx is not feasible during nasopharyngeal or clival surgery. We describe an alternative placement against the lateral nasal wall, especially suitable during clival or nasopharyngeal surgery, particularly if a maxillary antrostomy or medial maxillectomy is not required as part of the surgery.
Methods
Following induction of general anesthesia, the nasal cavity is decongested with pledgets impregnated with a solution of 1:10,000 epinephrine. At the beginning of surgery, the pledgets are removed and the lateral nasal wall is infiltrated with a solution of lidocaine 1% with epinephrine 1/100,000. The sites corresponding to the incisions needed for flap harvesting may also be injected; however, it is prudent to avoid injecting in the vicinity of the flap’s vascular pedicle.
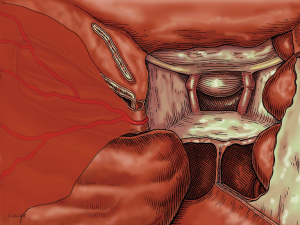
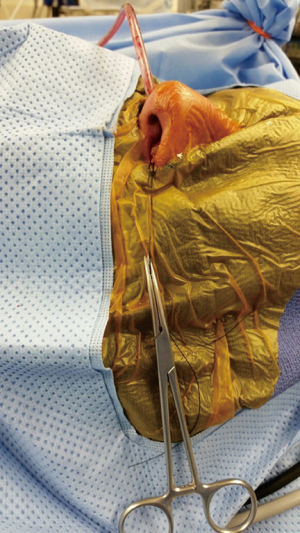
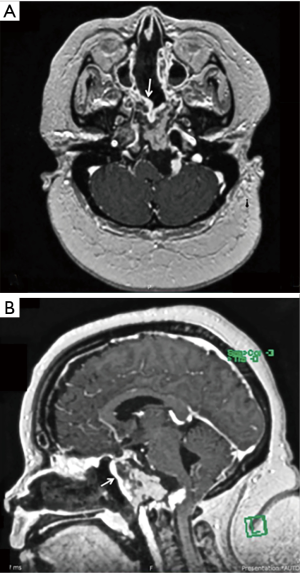
The anterior border of the posterior pedicle nasoseptal flap is brought out through the nostril and placed flat along the lateral nasal wall (Figure 1). A suture is placed through its anterior border, brought out through the nostril and clamped with a hemostat, which is allowed to hang freely from the nostril (Figure 2). The hemostat provides a counterweight that maintains the flap in an extended position along the lateral nasal wall, and; thus, out of the way of any instrumentation. Endoscope visualization should be used to guide the initial entry of instruments into the nasal cavity to avoid injury to the flap. However, once inside the flap is held against the lateral nasal wall and kept out of the way by the endoscope (right side) or the instrument (left) shaft. Placement against the lateral wall better emulates the flap’s original anatomical position. Clinically, this has translated in less congestion and less tendency for the flap to roll and adhere to itself (periosteal side) (Figure 3).
Results
We have used this technique in over 23 cases with no compromise to flap viability and no cerebrospinal fluid (CSF) leaks. However, the cases involved in this series were mostly nasopharyngectomy and clivectomy surgeries and, therefore, mostly did not breach dura. These cases were a mix of primary and revision surgeries and did involve patients who had recurred after radiation treatment. Pathologies included chordoma, chondrosarcoma, meningioma and nasopharyngeal carcinoma. The flap was suspended along the lateral nasal wall via a suture attached to a hemostat for between 2 to 9 hours.
Conclusions
The posterior pedicle nasoseptal flap is a versatile and robust flap with a large surface area that may be used to cover large skull base defects including clival and nasopharyngeal defects. As the posterior pedicle nasoseptal flap must be harvested before definitive extirpative surgery, it must be stored in a location that protects the flap from injury due to drills or instrumentation until it is ready for use. Traditionally, the posterior pedicle nasoseptal flap has been stored in the maxillary sinus, sphenoid sinus or nasopharynx. The nasopharynx and sphenoid sinuses are not viable storage options for nasopharyngeal or clival surgery and storage in any of these sites may result in congestion of the flap. Storing the flap along the lateral nasal wall overcomes both these problems and should be considered an option when using a posterior pedicle nasoseptal flap:
- Placing the posterior pedicle nasoseptal flap in the maxillary or sphenoid sinus or the nasopharynx during endoscopic skull base surgery causes congestion of the flap, risking its viability;
- Placement of the nasoseptal flap in the sphenoid sinus or nasopharynx is not possible during clival or nasopharyngeal surgery;
- Placing the nasoseptal flap along the lateral nasal wall during clival or nasopharyngeal surgery avoids congestion and emulates the original anatomic position of the flap.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ajo.2018.02.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). The patient involved in the photo gave written and informed consent for photographs to be taken and used in publications.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kassam AB, Thomas A, Carrau RL, et al. Endoscopic reconstruction of the cranial base using a pedicled nasoseptal flap. Neurosurgery 2008;63:ONS44-52; discussion ONS52-3.
- Hadad G, Bassagaisteguy L, Carrau R, et al. A novel reconstructive technique after endoscopic expanded endonasal approaches: vascular pedicle nasoseptal flap. Laryngoscope 2006;116:1882-6. [Crossref] [PubMed]
- Pinheiro-Neto CD, Prevedello DM, Carrau RL, et al. Improving the design of the pedicled nasoseptal flap for skull base reconstruction: a radioanatomic study. Laryngoscope 2007;117:1560-9. [Crossref] [PubMed]
Cite this article as: Campbell RG, Otto BA, Prevedello DM, Carrau RL. How I do it: modification of the posterior pedicled nasoseptal flap for clival and nasopharyngeal surgery. Aust J Otolaryngol 2018;1:13.


